Summaries by Nathan Elliott. Formatting and editing by Madeline Rizzo
| On Demand | Day One | Day Two | Day Three |
|---|

Civitas Networks for Health® is a national collaborative comprised of member organizations working to use health information exchange, health data, and multi-stakeholder, cross-sector approaches to improve health.
We’re in San Antonio this year for the Civitas Networks for Health 2022 Annual Conference. Join us over the upcoming days as we recap selected sessions from this year’s events! In this installment, we recap some of our favorite on-demand sessions that were available before the live conference.
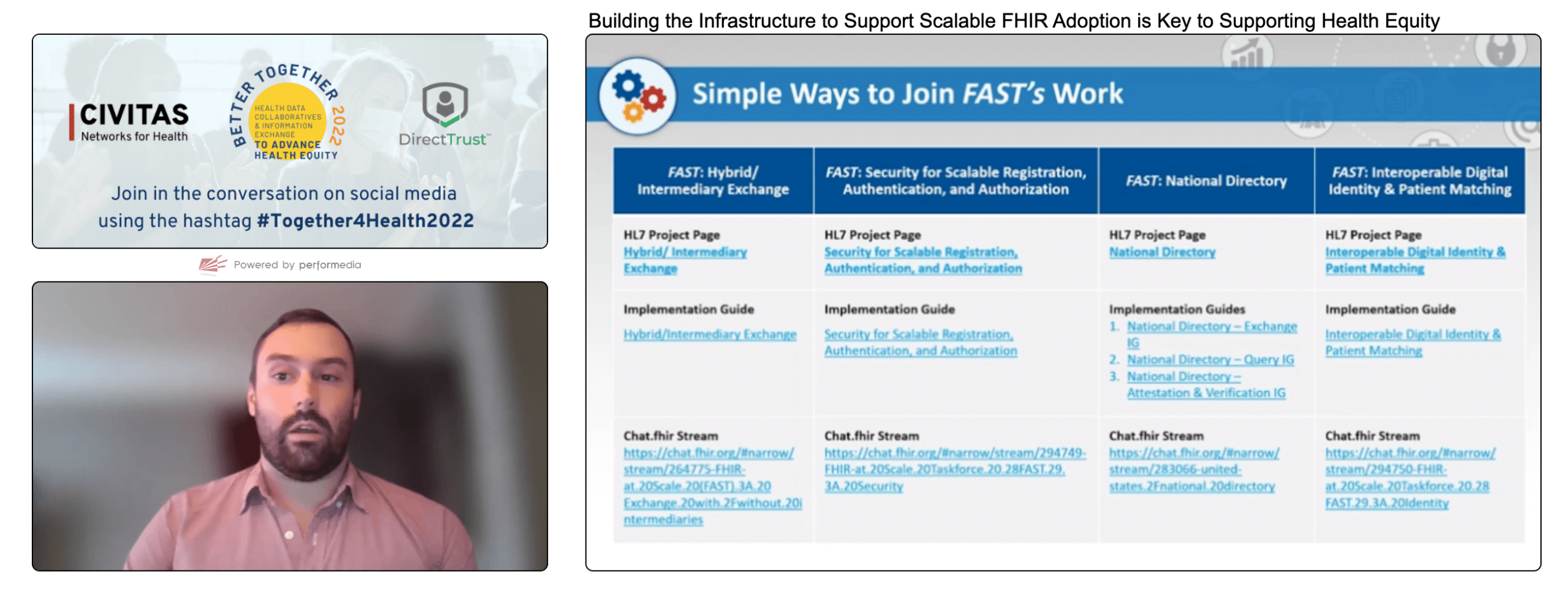
Building the Infrastructure to Support Scalable FHIR Adoption is Key to Supporting Health Equity

- Presenter: Alex Kontur
- Overview: ONC’s Alex Kontur guides audience members through the recent launch of the FAST Accelerator and its work to produce its 2022 Implementation Guides on security, identity management, a national provider directory, and intermediary exchange protocols.
In March 2022, the FHIR at Scale Taskforce (FAST) officially became one of the ONC’s Accelerator programs. The HL7 FAST Accelerator program, whose purpose is to establish a durable community for addressing ecosystem-wide barriers to using FHIR to enable interoperability at a national scale, is working to collect and solve large-scale problems identified by the other Accelerators (Da Vinci, Vulcan, Gravity Project, Argonaut Project, etc.).
Since launching in March, the FAST Accelerator community has spent some time defining policies, funding mechanisms, operating guidelines, establishing steering committees, and developing a PMO. Despite the name change and structural enhancements, many of the initiatives of the FAST community remain the same, including completing and publishing implementation guides (IGs). The FAST Accelerator community has been working on the following IGs this year:
Security Implementation Guide
This guide aims to define security standards that allow organizations to become trusted within a national network and make the process and experience of finding data sources and linking to them predictable and consistent. Kontur noted that CommonWell and Carequality have begun to include these protocols in their own FHIR implementation guides. The guide includes:
- Discover server support for UDAP workflows
- Dynamic client registration
- Certificate-based authentication
- OAuth 2.0 authorization flows for consumer-facing and B2B applications
Identity/Patient Matching Implementation Guide
This guide aims to provide national standards for patient data and FHIR functionality to assist with more efficient and accurate matching operations. The guide includes:
- Best practices for identity verification
- Guidance for patient matching workflows, including use of FHIR $match operation/li>
- Considerations for match scoring
- Requirements for digital identifiers
Directory Implementation Guide
This guide aims to define a core set of data about providers that can be used by intermediaries and value-add organizations to serve up consistent, timely, updated, and verified essential information for the national community. The intent is not to provide a directory that is accessed in real-time by consumers but to provide a reference data set for entities that provide tools and information to end-users. The guide is based upon:
- Developing a data model and API for a single national source of truth directory
- Defining APIs for local directories leveraging national directory data
- Defining processes for attestation and verification
Exchange Implementation Guide
This guide aims to define workflows for routing FHIR transactions through an intermediary. At this time, the guide is limited in scope and does not account for all scenarios, but it is a place to start. The guide considers a primary scenario where originating systems might be unaware of the intermediary in the transaction. Additional work will need to be done for scenarios where intermediaries do more than route transactions, such as hosting an authorization server.
The FAST Accelerator’s implementation guides are in varying states of completion at this time and are either published or will be published in the coming months. Kontur invited the audience to participate in the FAST Accelerator’s work. Questions can be posed at chat.fhir.org, and participation is encouraged by joining the listserv and the FAST Accelerator group on LinkedIn.
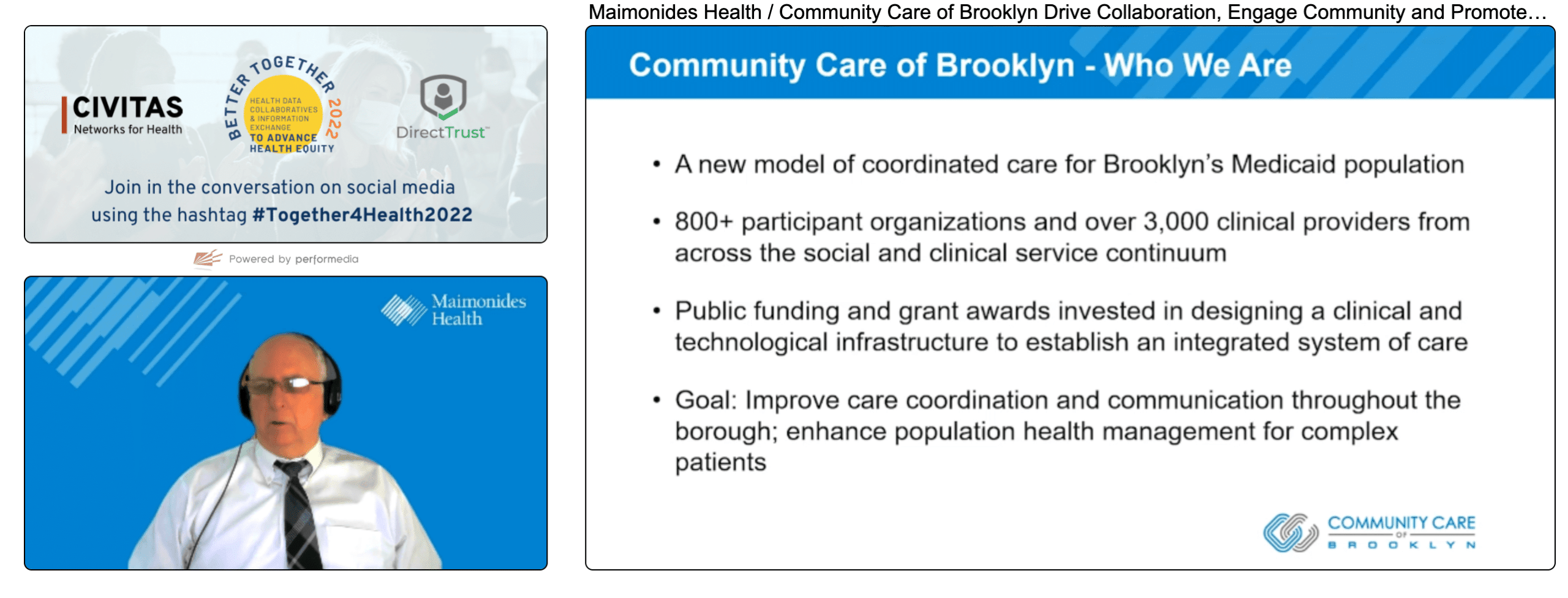
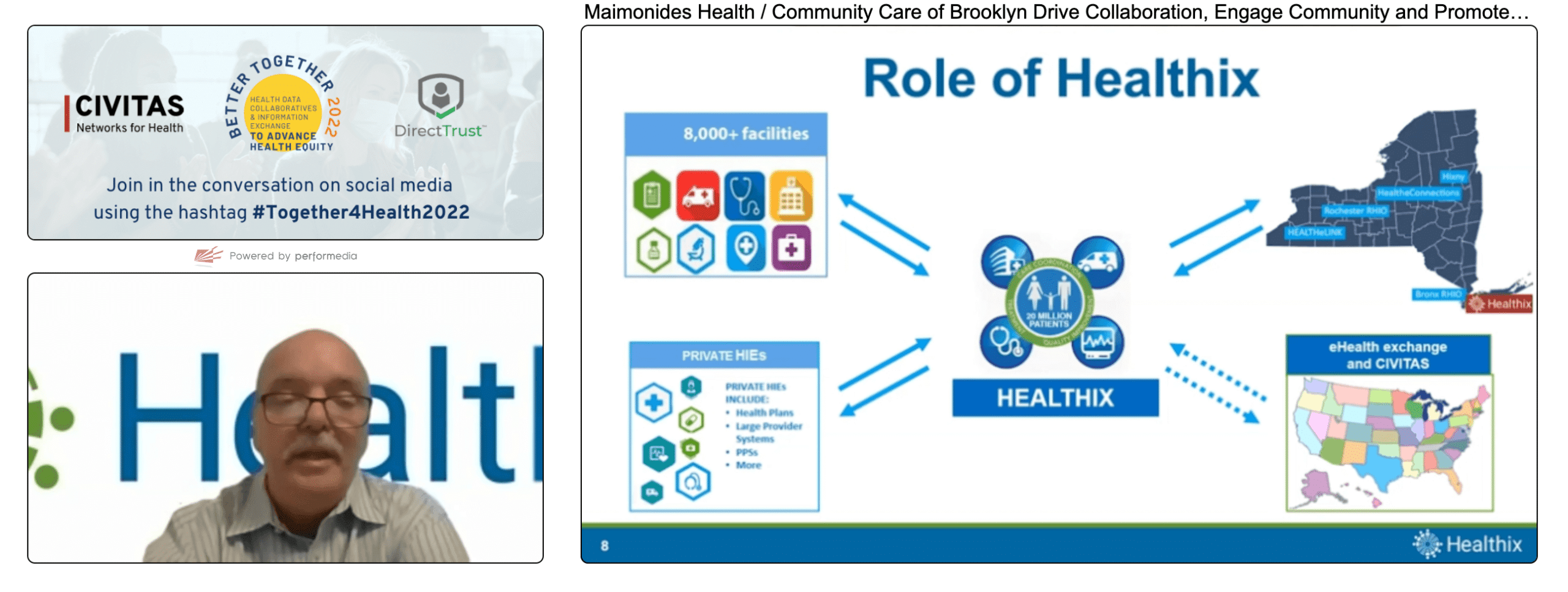
Maimonides Health / Community Care of Brooklyn Drive Collaboration, Engage Community and Promote Health Equity During COVID19 Pandemic
- Presenters:
- Michael Carberry, CIO for Population Health, Maimonides Health
- Brian Pisano, Manager, IT Implementation and Support, Maimonides Health
- Nick VanDuyne, Senior Vice President, CIO, Healthix
- Overview: Michael Carberry, Brian Pisano, and Nick VanDuyne led viewers through the history of Brooklyn public health organizations’ ability to turn existing but incomplete HIE data into a text message campaign that directly improved COVID-19 testing rates in the Brooklyn community.
This panel presented an overview of a grant-funded effort between Brooklyn Communities Collaborative, Community Care of Brooklyn (800+ participant organizations and over 3,000 providers), Community Care of Brooklyn IPA, and Brooklyn Health Home.
From June through November 2020, an average baseline of about 17,000 COVID-19 tests per month were performed in Brooklyn. In December 2020, Maimonides Population Health entered into a one-year grant with the NY Department of Health and Mental Hygiene to increase COVID-19 testing by at least 20% over the baseline, to approximately 21,000 completed monthly tests.
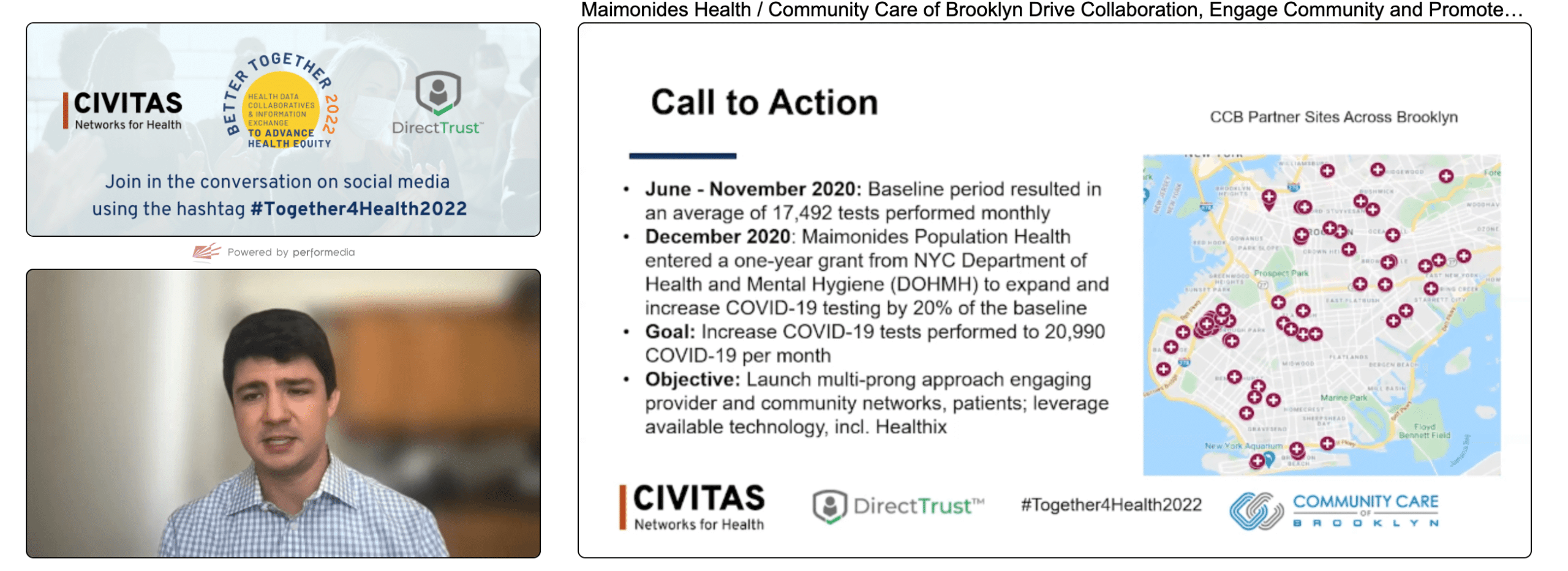
The collaboration used data from Healthix, the largest public HIE in New York, to identify what public health officials considered “hotspots” as the COVID-19 pandemic emerged and evolved. Such hotspots include Brooklyn areas with low testing rates, low vaccination rates, and high infection rates. These hotspots became focus areas for communicating with providers and directly with patients to improve awareness of testing sites and provider availability.
In addition to facilitating relationship-building between partner entities and delivering personal protective equipment (PPE) from New York City’s stockpile of supplies, Community Care of Brooklyn activated Participatory Action Research youth researchers to survey over 1,600 Brooklyn residents to assess concerns and barriers to public health responses in the winter of 2020. Survey responses showed that about 40% of residents were open to vaccination and testing, but 60% were not.
Based on these results and related input, program leadership designed an outreach strategy leveraging AWS Chat Bot technology to directly engage with the community through text messages. Throughout the grant period, over 330,000 text messages were delivered. Messages encouraged recipients to get tested and delivered educational resources to encourage proactive behavior in the community.
An AWS Professional Services team customized the SMS-based chatbot services based on the following technologies:
- Amazon Pinpoint: A highly scalable and globally distributed SMS service
- Amazon Lex: A service for building conversational interfaces using voice and text
- Amazon Connect: An omnichannel cloud contact center that directly connects members to managed call centers and other resources
The messages were designed as “Wellness Check In” style messages both in English and Spanish. Program leaders found that the largest barrier to project success was missing and inconsistent code values for indicating COVID-19 status. Some providers are still not providing codes today. This variability required “wild card” data searches to identify patients, which are still in use today. Efforts to standardize the use of disease-related codes are still underway.
Many Brooklyn residents are underserved and difficult to reach through traditional means. Overall, program leaders felt that the use of data, the Participatory Action Research team’s survey capabilities, and existing direct-to-member communication made the project successful.
Changing Our Approach Together: How We Can Move the Needle on Interoperability with Quick Wins

- Presenters:
- Theresa Bell, Cofounder, President & Chief Technology Officer, Kno2
- Carrie O’Connell, RN, Sr Director, Clinical Strategy, WellSky
- Peter Schoch, MD, Senior Vice President of Population Health & President of the Florida Hospital Physician Network, Advent Health System
- Travis White, SVP of Market Strategy & Adoption, Kno2
- Overview: Theresa Bell led the panel through a series of questions aimed at articulating steps providers and healthcare professionals can take to accelerate the value of expanded SDOH data.
Theresa Bell led the panel through a series of questions aimed at articulating steps that providers and healthcare professionals can take now to accelerate the value of expanded SDOH data in addressing what has historically been out-of-reach patient non-compliance. Panelists took turns providing their recommendations, perhaps most notably the significance of the mind shift from viewing healthcare as identifying and treating disease to understanding that an estimated 80% of health and wellbeing is driven by factors outside of what healthcare is designed to address.
Thus far, reimbursement and payment programs have been designed to review specific indicators of disease and then treat those diseases. Unfortunately, payment models do not tend to focus on paying providers or hospitals for doing things like improving air quality in a patient’s home or ensuring that they have reliable transportation. Yet it is these factors that directly affect patients’ ability or willingness to follow medical directions to improve their health. A patient might have diabetes, but there can be multiple additional factors that make consistently following medical advice impossible to treat that diabetes.

Eighty percent of health is determined by barriers to accessing appropriate and available services in a community, behavioral health factors, effects of poverty, and such factors as a patient’s home life and stability of relationships. While changing payment programs and incentives will require a greater effort, the panelists felt that smaller-scale steps could be taken to begin influencing the use of data to respond to external factors to health. These steps include:
- Recognizing and calling attention to unconscious biases against SDOH (or “post-acute”) data, such as providers’ tendency to dismiss data provided by home care services or ignore assessments and conducting their own as the “truth” in a hospital or office setting.
- Using available technology to more consistently capture SDOH data and mitigate at least some of the human biases that enter into how screening questions are asked.
- Using the most relevant data available within providers’ existing workflows and not coming up with one-off solutions that leverage lots of data but place it outside of providers’ preferred (efficient) processes.
In the future, the panelists hope that we can expand the use of technology and SDOH data to empower clinicians to place orders for care-related interventions beyond traditional diagnostics and treatments. They imagine a future where a clinician can order new air filters or have a new air conditioner installed in a patient’s home, as well as more efficiently provide community services access to patients struggling with food insecurity.
It is essential to facilitate health improvements to not only know if a patient has a large amount of expired food in their refrigerator or appears to have a mold problem but also have the ability and financial backing to do something about it. We need to accelerate progress to get to that point, which means doing a better job of using data to justify the systemic changes necessary to realize such a future.
| On Demand | Day One | Day Two | Day Three |
|---|
Thank you for joining us for these sessions at Civitas! Stay tuned for more recaps!
J2 Interactive is an award-winning software development and IT consulting firm specializing in customized solutions for hospitals, labs, research institutions, and health information exchanges.
Our approach to design and development is rooted in a fundamental belief that systems succeed or fail based on how well they serve the people who depend upon them. Drop us a line to learn more.