The first keynote session of the READY 2025 conference provided an in-depth examination of Artificial Intelligence’s (AI) multifaceted influence on the healthcare sector, encompassing discussions on potential job displacement, data utilization strategies, operational efficiencies, and the evolving professional roles within healthcare.
Terry Ragon, founder of InterSystems, opened by addressing one of the top concerns associated with advancing AI technologies: job loss or displacement.
Ragon acknowledged the potential for AI-driven job displacement while concurrently asserting that historical technological advancements have consistently led to enhanced productivity and the creation of more engaging roles in the long term, citing Electronic Medical Records (EMRs) as a precedent that did not result in a net reduction of jobs.
Ragon underscored the persistent challenge of AI hallucination, emphasizing the imperative of providing source links for AI-generated responses and reiterating AI’s role as an assistive tool, with ultimate human accountability. He further noted that pilot programs suggest the disabling of certain question types to avoid dictating professional methodologies.
The burgeoning trend of computing as a service, globally provisioned by InterSystems, was presented as a significant paradigm shift fostering growth and innovation.
Ragon concluded by defining his organization’s core identity as a creative technology partner committed to excellence and client success, sustained by a culture that cultivates innovation to attract similarly innovative individuals.
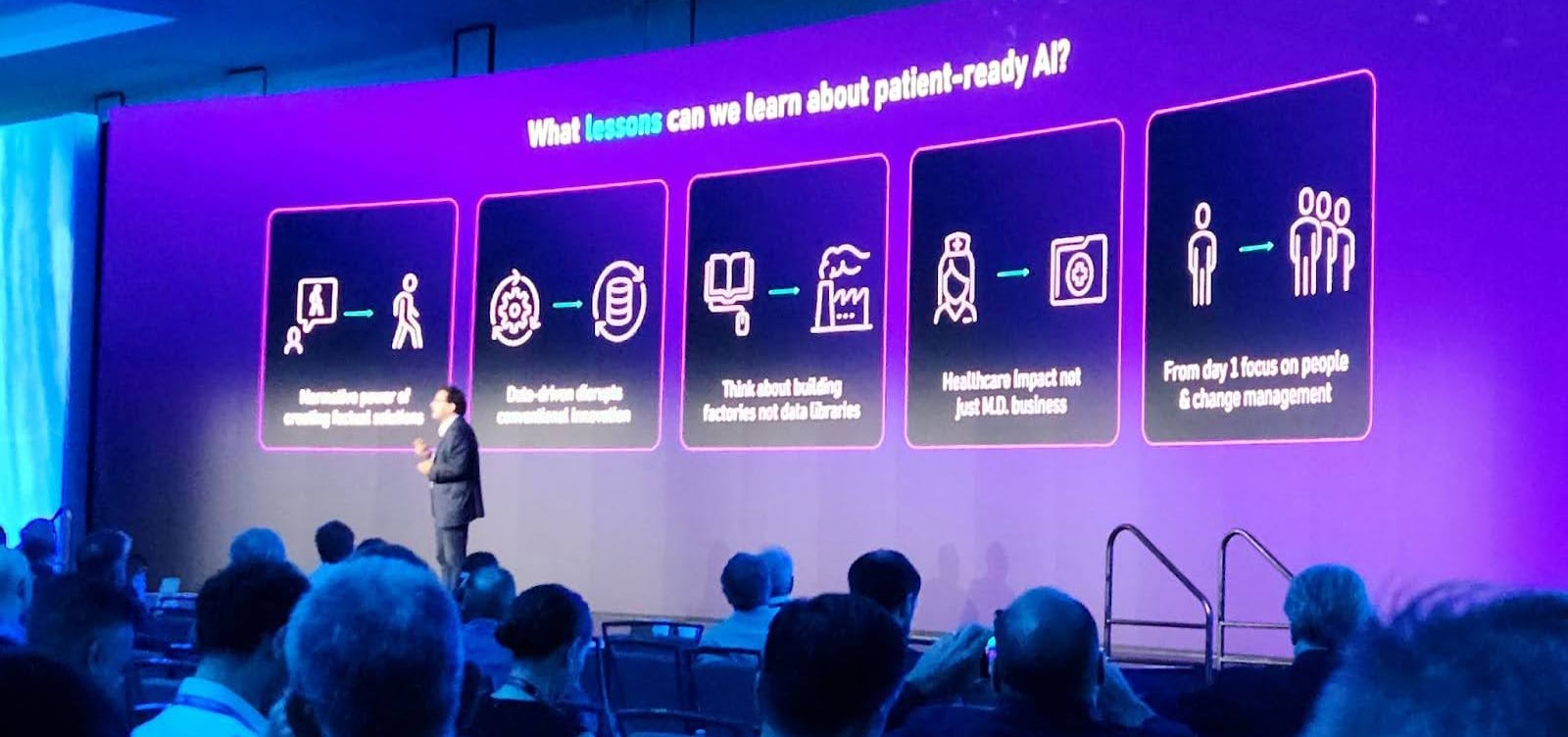
Aldo Faisal concentrated on the development of AI systems capable of autonomous problem-solving and data-driven learning.
He presented a cholera case study at the intersection of public health and data visualization, elaborating on modern case studies that demonstrate how administrative, retail, and movement assessment data can predict outcomes with greater speed, cost efficiency, and accuracy than conventional methods. Specifically, changes in retail behavior (changes in grocery shopping due to symptoms of bloating) were shown to predict ovarian cancer eight months prior to symptom onset, and administrative healthcare updates and actions recorded in hospital systems predicted unplanned hospitalizations with an 80% accuracy rate.
Faisal introduced the concept of “agentic AI,” characterized by its capacity for independent decision-making and path selection. He stressed that integrating generative AI into agencies requires a focus on the sociological dimensions of the problem, rather than solely on technological, legal, or clinical aspects.
He also emphasized the critical need for comprehensive data integration and improved decision support, conceptualizing AI as a “sherpa” guiding users toward realizing AI’s full potential.
Faisal concluded by highlighting that healthcare impact extends beyond medical data, thereby requiring the integration of diverse data sources and a foundational focus on change management from inception.
Kari Hedges challenged the audience to accelerate the adoption of AI, questioning the healthcare system’s preparedness for the requisite changes to actualize the AI examples she gave in this session. She raised concerns regarding the usability of existing electronic data, noting the continued reliance on antiquated methods such as faxes and compact discs. Hedges articulated a vision wherein healthcare professionals possess real-time awareness of care delivery locations, a patient’s progression within their care pathway, payment status, and the ability to obtain immediate prior authorizations.
According to Hedges, only 35% of prior authorizations are immediate. Through a personal narrative concerning her mother’s post-surgical difficulties with data exchange and her reliance on paper or CD-based transfer of information to another care facility and provider, Hedges underscored the paramount importance of patient-centricity, fostering interprofessional communication and collaboration, and surmounting security and other perceived barriers to change.
She detailed Blue Cross Blue Shield’s (BCBS) interoperability initiatives, observing that 33 independent BCBS plans now facilitate real-time clinical data exchange for patients and providers. This endeavor aims to mitigate paper-based processes and reallocate resources from administrative tasks to clinically meaningful work. A prior authorization study conducted by BCBS revealed that 84% of prior authorizations were in fact not mandatory, and current efforts aim to achieve 80% real-time prior authorizations from the present 20%, thereby improving timeliness by one-third. Another plan in Florida achieved a 96% electronic submission rate for prior authorizations, with the goal of expedited approvals while the patient remains in the provider’s office.

A Panel Discussion, facilitated by Christina Farr, offered a few perspectives on the future of AI in healthcare.
Jennifer Eaton forecasted genuine patient engagement with AI within the ensuing five years, underscoring the need to extract actionable insights from the burgeoning volume of data. She enumerated various use cases, including call center chatbots and care coordination, viewing AI as a long-term catalyst for cost reduction and health improvement, particularly for aging-in-place and home care models. She posited that AI will achieve sufficient sophistication to diminish the necessity of direct interaction with live representatives, offering proactive, personalized communications based on patient interests.
Tim Ferris envisioned nearly entirely AI-driven interactions with the healthcare system for routine tasks, while complex tasks such as care coordination would require a longer transition period. He estimated that 30-40% of health transactions constitute rote tasks. Within five years, he anticipated the presence of a “third listening or cognitive entity” during physician visits, offering recommendations and potentially evaluating provider adherence. He suggested that patient demand and the imperative to treat a larger patient population more rapidly will drive AI adoption, supplementing physician judgment with decision support tools. He also observed the growing trend of individuals using generative AI for medical information (e.g., ChatGPT).
Don Woodlock focused on the immediate 3-5 year horizon, predicting that AI’s initial application would be to the administrative facets of provider work, aiming to prevent burnout and foster trust, ultimately progressing toward clinical engagement.
Scott Gnau emphasized the expansion of AI beyond solely clinical data to encompass lifestyle data, thereby facilitating proactive lifestyle management and prevention through pertinent patient conversations outside of illness.
Woodlock then noted that the uptake of AI interventions is substantially higher when presented to patients or providers within the established system (80% efficacy) compared to unsolicited outreach (15% efficacy).
Ferris highlighted the central challenge of behavior modification, specifically the absence of aligned financial incentives for individuals to improve their health, given that 70-80% of healthcare costs are predictable. He proposed that AI could revolutionize health insurance by establishing incentives for self-care, thereby simplifying the currently intricate insurance structure.
Eaton stressed the importance of individualized care, advocating for a transition beyond fee-for-service models to population-level thinking while concurrently addressing unique patient needs, including transportation or food desert issues.
Woodlock pointed out the incongruity between healthcare being a frequently searched online topic and the low adherence to preventive care, such as mammograms.
Regarding the impact of efficiency, Woodlock asserted that mitigating provider stress and enhancing job fulfillment are critical to attracting more providers and reducing burnout. Ferris added that AI can alleviate cognitive load by identifying clinically relevant information embedded within data, such as family histories, thereby affording providers more time for empathetic patient interaction. The discussion also addressed the evolving skill sets required for medical professionals, with Ferris noting that medical schools are increasingly valuing backgrounds in the humanities alongside scientific disciplines. Eaton foresaw a transformation in how nurses interact with patients, moving beyond mere medical examinations.
Gnau predicted that AI would ultimately reduce healthcare costs and overcome existing barriers, emphasizing the necessity of clean data to minimize AI hallucinations. Woodlock observed that successful AI studies, including those mentioned by Aldo Faisal earlier in the session, frequently involve contained populations with robust data fidelity, underscoring the need for comparable data quality for broader AI implementation. Ferris discussed the financial challenges faced by providers and the imperative to reconfigure existing technology, advocating for the identification of early adopters and leveraging their success stories to drive broader adoption.
The panel concluded with each panelist’s thoughts on AI’s potential for “big ideas” or greatest impact for the near-term future of healthcare:
- Gnau: Automating appointment scheduling through AI.
- Woodlock: Streamlining the complexity of prior authorization processes.
- Ferris: Achieving millisecond-level responses for prior authorization based on appropriateness criteria.
- Eaton: Providing patient-friendly summaries of clinical data and test results, integrating all information for clear comprehension on a self-service basis, without awaiting provider interpretation or the next appointment with a healthcare provider.

