
Clinical terminologies and clinical classification systems represent two coding schemas used in healthcare. Chances are your organization uses both, and how you manage them might need a tune-up.
Terminology in Healthcare – Different from what you expect
Clinical terminology is different from medical terminology. Medical Terminology refers to the vocabulary that medical professionals use to describe the body—what it does, diseases that impact it, and procedures to correct it —enabling precise communication among practitioners.
Clinical terminology systems are used to code the entire healthcare domain, from procedure to diagnosis and beyond. They function as a common reference system that uses compositional grammar concepts (conversation words) that can be coded and queried. Terminology systems personalize medicine such that everyone is speaking the same language about a patient in the exam room and the billing office. These systems also provide support for clinical trials and research across multiple organizations. Additionally, they offer semantic interoperability for sharing data easily and accurately.
Healthcare Terminology, Explained
In healthcare, terminology is much more complicated than in other fields. This complexity is because there needs to be a group of expressions for a large number of permutations and combinations (to borrow a mathematical term) of clinical diagnoses and treatments.
If you think of “fracture of the proximal tibia (shinbone)” as one form of many possible tibial injuries, imagine how many sets of words are needed to describe all the different types of injuries and conditions across the 206 bones in the human skeleton (and the skeleton is just a subset of the human anatomy).
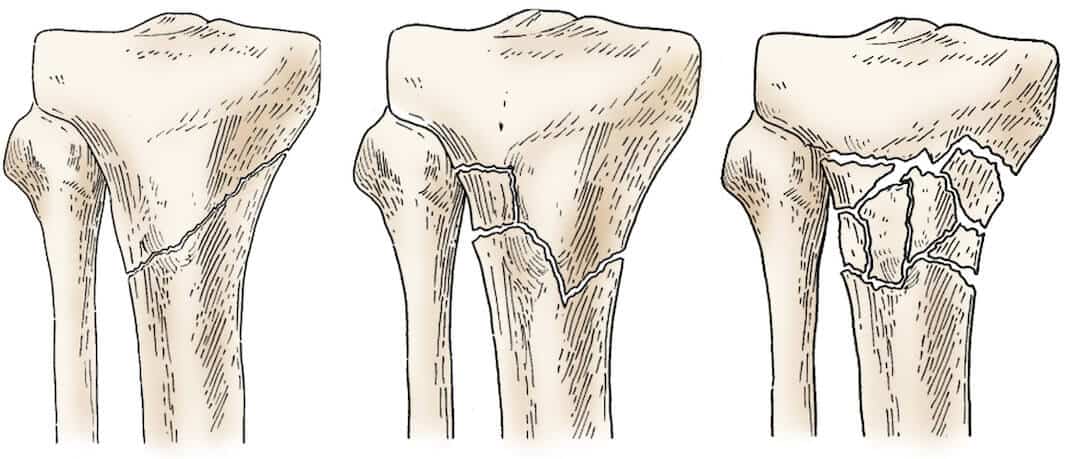
Source: OrthoInfo.com
When there are thousands upon thousands of sets like these, words alone aren’t manageable. You need numbered codes, and they must be arranged in a hierarchy. Plus, you’ll need to build out hierarchies for different types of users.
Different Codes for Different End Users
Not all functional areas and roles within a health system require the same level of precision when it comes to identifiers for diagnoses and treatments:
1. A physician needs to precisely document a visit in an EMR. They will use a problem list and diagnosis codes. For example, SNOMED CT or customized homegrown codes
2. A lab test is performed during the visit. Codes are assigned and associated with these items. For example, LOINC
3. The physician orders a medication. For example, RxNorm
4. A billing/coding specialist would use documentation from a provider and assign codes to appropriately bill for the visit. For example, CPT and ICD-10
5. A call center agent, for example, is best off viewing plain English information in a CRM system when talking to a patient (“Oh yes, I see that you were treated for your broken leg last August”)
6. Integration data coming across the EMR from outside sources containing SNOMED, LOINC, NDC, RxNorm, and local codes
As you can see, differing levels of precision have given rise to different coding systems.
Similar Names, Different Use Case: Clinical Terminology vs. Clinical Care Classification
Broadly, the coding systems discussed above fall into these buckets:
- Clinical terminology codes—Codes that cover the entire domain of healthcare terms, such as SNOMED CT
- Clinical care classification codes—Codes that cover specific diseases, diagnoses, lab reports, procedures, or meds. Examples include NDC codes for medications and CPT for procedures/services
In an HIE or health system, there needs to be an exchange of data among applications—both within and across these buckets. Systems have to determine the best matches among disparate coding sets. To achieve this, your organization must build and maintain data maps, then load the results into an interoperability platform such as InterSystems’ HealthShare.
Learn about our Managed Terminology Services for your HIE
Clinical Terminology
Clinical terminology, as its name implies, exists primarily for use by caregivers.
Having agreed-upon codes in an EHR system is important for ensuring a standardized treatment or set of treatment options for a specific medical issue.
Assume two patients come into the hospital on different days. Each complains of acute pain in their right leg and has a nearly identical closed fracture in the upper end of the right tibia. For consistency, the issue observed for both patients should be coded the same way in the EHR system.
The terminology standard in clinical applications is SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms).
Just as Google uses natural language processing (NLP) to apply meaning to the words in this blog post, SNOMED CT uses NLP to generate codes from medical text. Clinical expressions are automatically coded in the background without users needing to know said codes.
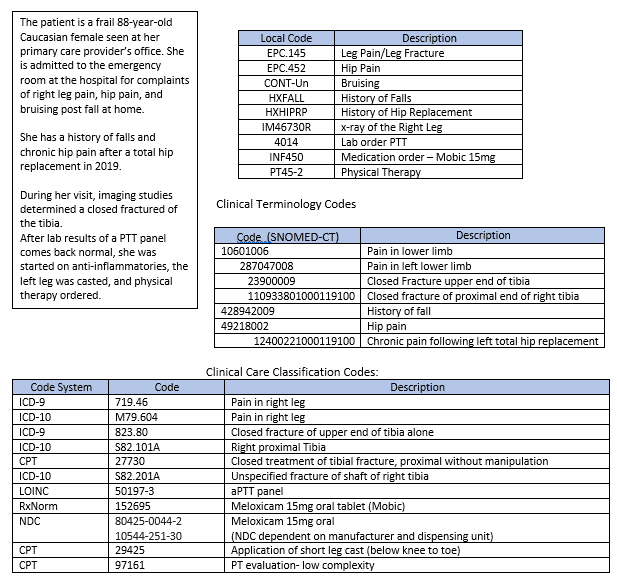
SNOMED uses what are called “concept codes.” Concepts are a clinical idea with a unique identifier. The concepts themselves (e.g., nausea and vomiting) are in clinicians’ transcriptions while the corresponding codes (e.g., 16932000) provide a unique identifier. The principle is based on one code per meaning, one meaning per code. Other examples of concept codes are:
- 23900009: Closed fracture of upper end of tibia (disorder)
- 10925201000119100: Closed fracture of proximal end of right tibia (disorder)
As with other healthcare data elements, terminology should be normalized among different clinical and non-clinical systems to ensure as much uniformity as possible.
Clinical Care Classification Codes
As stated above, classifications refer to the codes that are used in healthcare environments for billing and accounting. They’re also used for statistical analysis and reporting but are NEVER used to document in EMRs.
Classification Codes: ICD-9 and ICD-10
International Classification of Diseases, Ninth Revision (IDC-9), and Tenth revision (IDC-10) are classifications.
Classification codes are important for billing the correct amount to patients. According to an article by Doug Klinger, CEO of Zelis Healthcare, medical bills are riddled with errors. Careful implementation of a terminology management system can mitigate the risk of errors.
ICD-9
The main format for ICD-9 codes is two or three digits to the left of a decimal point and one or more digits to the right.
Examples include:
- 823.80: Closed fracture of unspecified part of tibia alone
- 823.02: Closed fracture of upper end of fibula with tibia
ICD-10
ICD-10 codes include two or three alphanumeric characters to the left of a decimal point and two or more alphanumeric characters to the right.
Examples are:
- S82.101A: Unspecified fracture of upper end of right tibia, initial encounter for closed fracture
- 79.16: Closed reduction of fracture with internal fixation, tibia, and fibula
If you go to the Find-a-Code website and type in a search such as “fracture of tibia,” you’ll get an appreciation of just how many classification codes there are.
An ICD-9 diagnosis is equivalent to one or many (usually a sub-hierarchy) ICD-10 diagnoses. i.e., 729.5 (Pain in limb) is equivalent to M79.609 (Pain in unspecified limb). The latter is a sub-hierarchy that contains six specific diagnoses.
Current Procedural Terminology (CPT) Codes
While an ICD code identifies a diagnosis and describes a disease or medical condition, a CPT code describes what was done to the patient during the consultation, including diagnostic, laboratory, radiology, and surgical procedures.
Here is a detailed explanation of the difference between ICD and CPT codes.
There is a five-digit CPT code on each line item on the bills that patients and payers receive. A doctor will not receive payment from a payer, furthermore, unless a CPT code is listed on the claim form.
Here is a more in-depth look at CPT codes.
Managing Clinical Terminology and Classifications
As you can see from the above examples, there are a wide variety of code systems across systems. The alphanumeric identifier for “fracture of upper end of tibia” in one system may have nothing in common with the identifier in another.
A traditional way of managing the disparities across systems is with the use of spreadsheets. However, spreadsheets involve a lot of manual work. Throw local codes into the mix, and you can start to see the need for an easier solution.
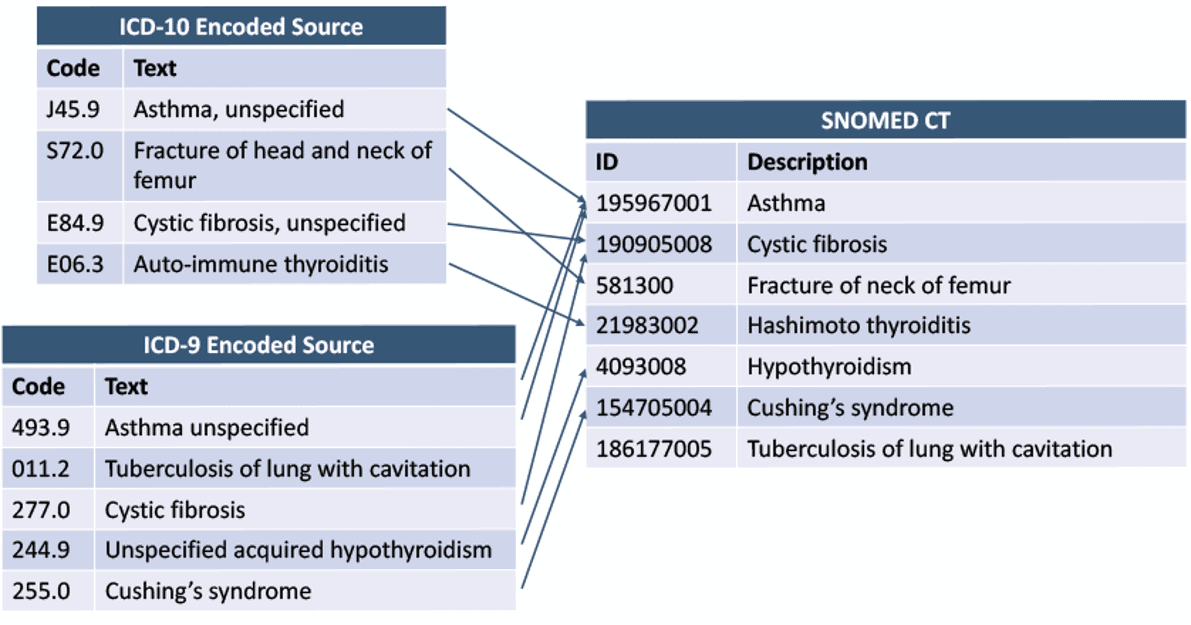
Source: SNOMED International
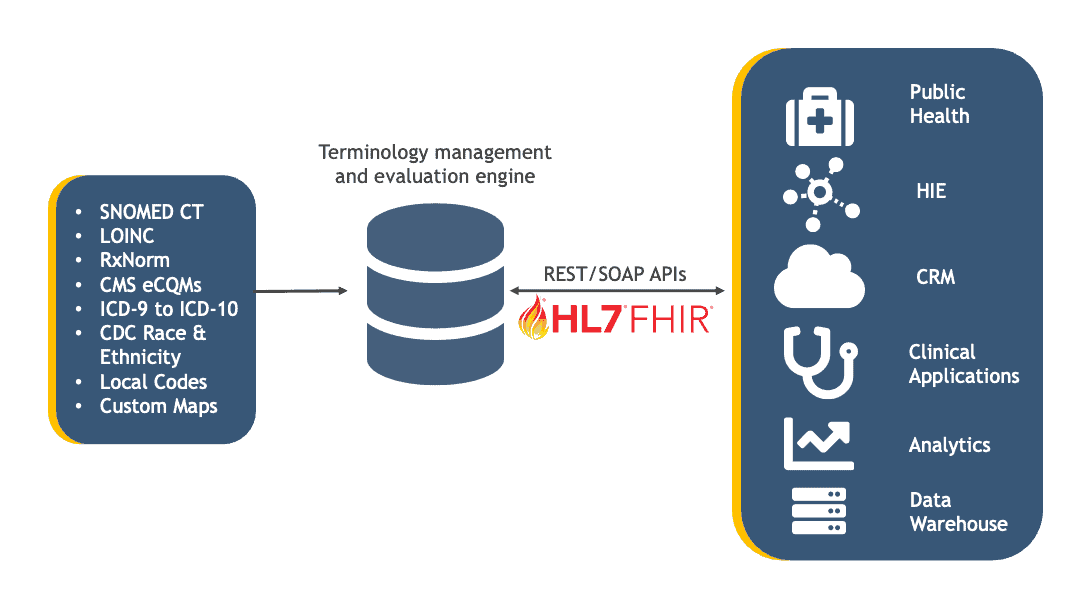
Setting up a terminology solution would shift manual processes to a highly automated and much less labor-intensive platform. Semantic services go beyond just the coding systems mentioned above. Libraries can include:
- SNOMED CT
- ICD-9
- ICD-10
- LOINC
- RxNorm
- CMS eCQMs
- MedDRA
- CVX/MVX
- CDC (demographics)
Clinical terminology management and the management of other coding systems include flowing normalized data into a number of different types of systems and environments using industry protocols, including FHIR. The diagram below shows examples of data types and target systems typical in J2’s Managed Terminology service.
In conclusion
Clinical terminology and classification are easy concepts to understand, but they’re complicated for an IT department to manage to scale. To reduce billing errors and clinical mishaps, healthcare organizations should be ready to retire spreadsheets and invest time and resources in a dedicated terminology solution.




