Summaries by Nathan Elliott. Formatting and editing by Madeline Rizzo
| On Demand | Day One | Day Two | Day Three |
|---|

Civitas Networks for Health® is a national collaborative comprised of member organizations working to use health information exchange, health data, and multi-stakeholder, cross-sector approaches to improve health.
We’re in San Antonio this year for the Civitas Networks for Health 2022 Annual Conference. Join us over the upcoming days as we recap selected sessions from this year’s events! In this installment, we recap some of our favorite Day Two sessions.
Health Equity by Design and the Evolving Health IT Landscape
- Date: Tuesday, August 23, 2022
- Presenter: Steven Posnack, MS, MHS, Deputy National Coordinator, Office of the National Coordinator for Health IT
- Overview: The ONC’s Deputy National Coordinator, Steven Posnack, discusses the office’s advice for prioritizing health equity and how the public can engage with the federal government to influence future policy. He also responds to a variety of questions from audience members.
Steven Posnack, Deputy National Coordinator at the Office of the National Coordinator for Health IT (ONC), gave a presentation on the federal government’s need and desire to engage the public and other stakeholders in advancing health equity. Part of the ONC’s role is to articulate success as it relates to informing new policy. Feedback from the field can help shape the next stage of regulatory processes. The ONC seeks to help everyone navigate the communications and relationships necessary to bring new ideas into the regulatory process.
Due to its limited budget, the ONC is looking across federal partners to act through sister agencies. Posnack feels like Medicaid is one of their biggest partnership opportunities. Posnack explained that he and his team are working with leaders to ensure that their missions are aligned with the ONC’s goals for the health IT community.
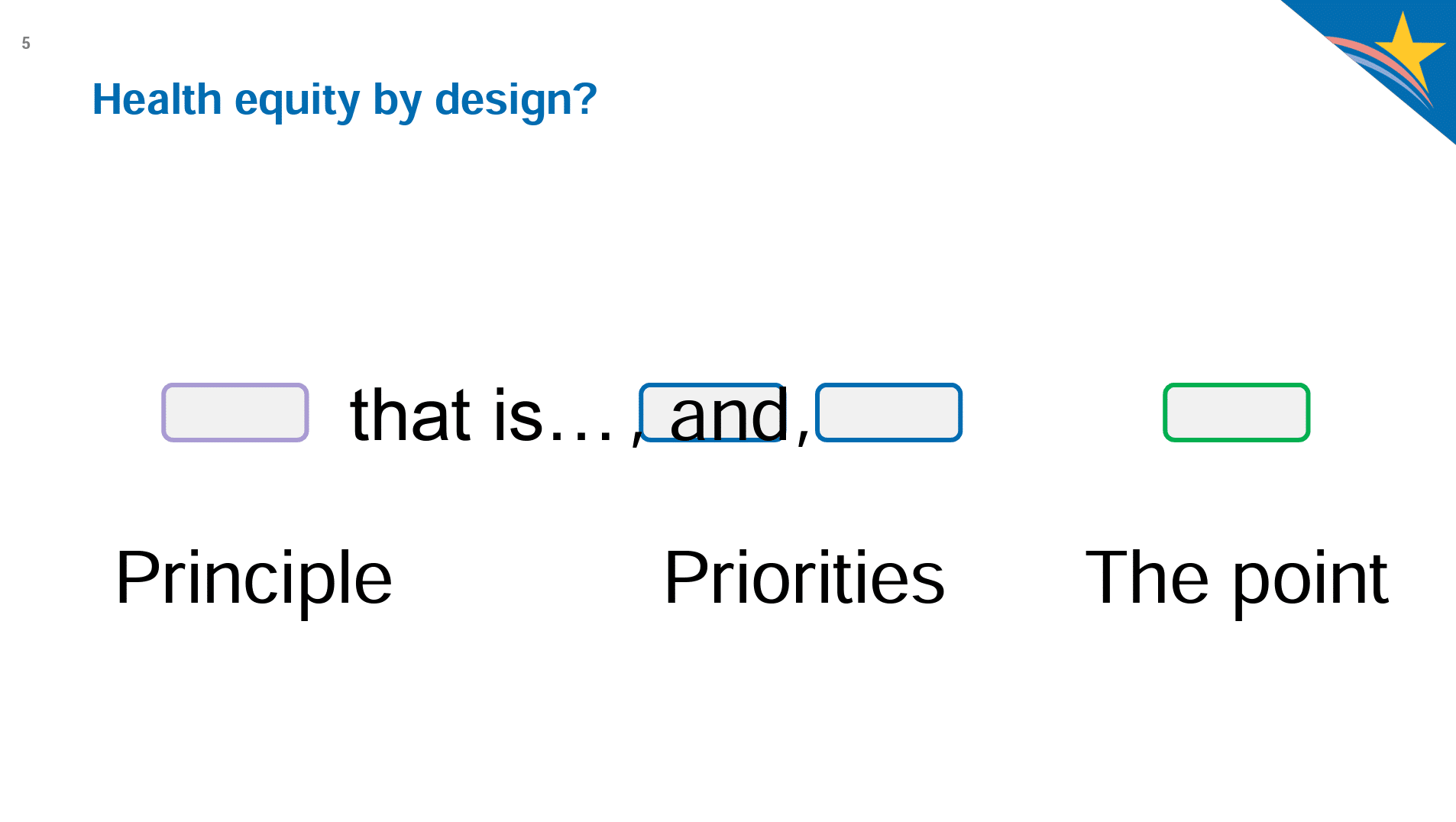 Perhaps Posnack’s most salient statement was that we often keep adding things to what we want to track and do with data. We put things like “and is accessible…” or “and is equitable…” at the end of our research or goal statements. But, doing it this way puts some of the most important topics into the “and” series at the end of our statements, which are then treated more like an afterthought and become less visible and less important. If we want health equity, we have to move it to the front and use those words first as a top priority. In other words, if health equity is important to us, we need to say it explicitly, not assume it or fold it in as an afterthought.
Perhaps Posnack’s most salient statement was that we often keep adding things to what we want to track and do with data. We put things like “and is accessible…” or “and is equitable…” at the end of our research or goal statements. But, doing it this way puts some of the most important topics into the “and” series at the end of our statements, which are then treated more like an afterthought and become less visible and less important. If we want health equity, we have to move it to the front and use those words first as a top priority. In other words, if health equity is important to us, we need to say it explicitly, not assume it or fold it in as an afterthought.
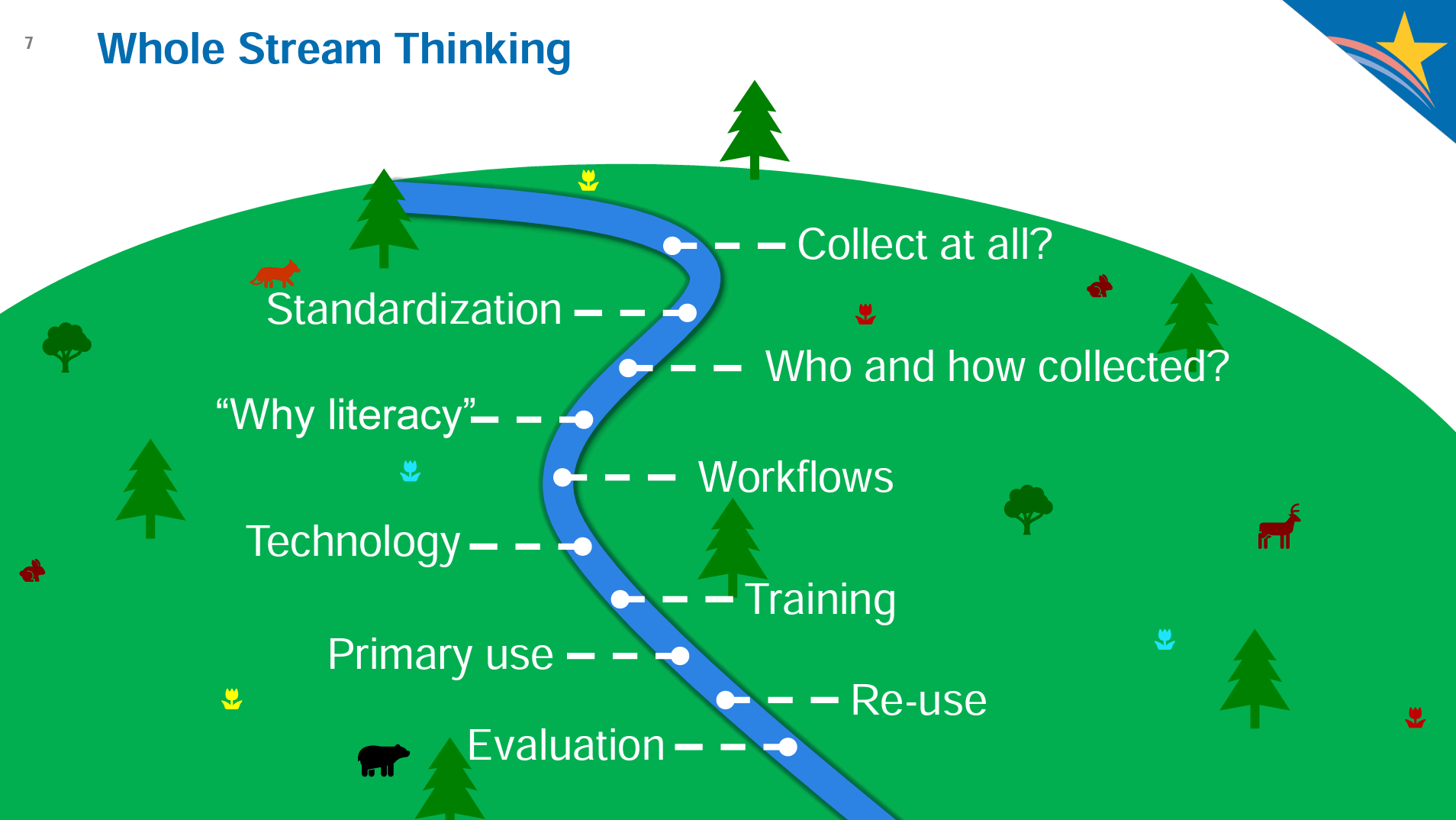 Posnack is excited about all of the data we are now capturing but also wanted audience members to think about how that data might be used or misused in the future. Clearly defining the data, why it is being collected, and providing context to reporting and analysis could help guide future data use. For this reason, we need to prioritize standardization, such as through the Gravity Project or efforts to standardize SDOH. We should think through not only data’s primary use but also its reuse potential and how we should evaluate whether the data and its collection practices are leading to the desired outcomes.
Posnack is excited about all of the data we are now capturing but also wanted audience members to think about how that data might be used or misused in the future. Clearly defining the data, why it is being collected, and providing context to reporting and analysis could help guide future data use. For this reason, we need to prioritize standardization, such as through the Gravity Project or efforts to standardize SDOH. We should think through not only data’s primary use but also its reuse potential and how we should evaluate whether the data and its collection practices are leading to the desired outcomes.
Some examples of the results of vague data strategies can include:
- Low adoption of race, ethnicity, language (REL) standards
- Lower priority given to referrals to social services
- Algorithms that perform differently
- Patient matching algorithms that do not account for circumstances of under-served communities
- Preventive care
- Lower priority to provide certain populations access to data
- Medical devices that perform differently
- Accessibility differences
Posnack then reviewed some of the programs through which the audience and the ONC interface, including TEFCA, LEAP (community-based referrals), PHIT, STAR HIE (demonstrates HIE impact on underserved populations), IDEAS, USCDI and standards coordination, certifications, and coordination at the state level in terms of Medicaid.
The ONC is interested in elevating HIEs and similar organizations and knows that audience members are actively building capacity, new connections, and collaborations. HIEs are in a unique position to establish benchmarks for performance at local and state levels.
The session then moved to Q&A.
One attendee asked about how social data fits into the ONC’s work. Posnack commented that, in the past, many people struggled with understanding how and why HIEs were important. At the time, IT adoption was the focus and the use cases (and their urgency) were not well articulated or understood. There has been a real evolution in the last five years, and different offices and agencies are not only seeing HIEs differently but are becoming more vocal about the need to understand patients and health factors outside of just the hospital or provider’s office. From a public service perspective, this is good to see and is motivating for staff.
An attendee asked about the ONC’s view of self-reported data. Posnack said that surveys used to be strictly paper-based. We are now able to engage patients in better ways through their phones. In addition to making sure we make data useful, we also need to make sure patients are health data literate, which is important to improving the quality of patient-generated health data. The ONC is currently working with other agencies to determine where and how they might be able to make positive contributions here. No specific targets or guidelines were offered, but the ONC is studying patterns.
 Posnack took a question about whether QHINs will be required to use certified technology or processes. He responded that the ONC has not yet explored getting into certification requirements. If they were to be involved, Posnack felt it would be most valuable for the ONC to participate in conformance testing for interoperability. The ONC might also assist with policy analysis to determine whether we need regulatory solutions to establish certification criteria, but additional discussions and decisions need to be made to make any statements about whether there is enough added benefit for the ONC to invest in these kinds of steps.
Posnack took a question about whether QHINs will be required to use certified technology or processes. He responded that the ONC has not yet explored getting into certification requirements. If they were to be involved, Posnack felt it would be most valuable for the ONC to participate in conformance testing for interoperability. The ONC might also assist with policy analysis to determine whether we need regulatory solutions to establish certification criteria, but additional discussions and decisions need to be made to make any statements about whether there is enough added benefit for the ONC to invest in these kinds of steps.
Another attendee asked about the move toward FHIR and, specifically, the amount of investment HIEs have made in standards like CCD/C-CDA. According to Posnack, the ONC sees FHIR adding the most value in new and less adopted use cases going forward. Organizations working to solve new use cases will likely begin by looking at FHIR. It will be some time before we transition away from the likes of CCD/C-CDA.
A question came in about the fact that we have millions of NPIs, 6,000 insurance companies, and over 400,000 apps. How does a provider or provider organization vet technology such as apps? Posnack responded by saying that if a provider uses an app themselves or for their practice, the expectation is that they will do their due diligence. There is no expectation, however, that providers or provider organizations must also vet the myriad apps available to patients. Patients are expected to do their own validation before using any of them. It is perfectly acceptable for providers and provider organizations to introduce warning pages and reminders before a patient authorizes a given app to receive data from a provider’s system (note: the app does not reach in to extract data). Risk factors are considered low in this scenario, in part because each person has to authenticate themselves with credentials that the provider organization has supplied.
Posnack took a final question about the Supreme Court’s recent Dobbs decision and its effect on sharing sensitive women’s health data across state lines. The attendee asked whether there is any guidance on information blocking as it pertains to this. In response, Posnack made it clear that the ONC is acutely aware of this issue. Many of us took for granted the policy layer that previously existed, but it now puts this and related scenarios into the limelight. While information blocking language does provide some coverage for this type of issue and there have been requests to clarify where the rule affects this type of information, there is still a significant amount of review taking place. Since information blocking is still a relatively new legal paradigm (implemented in 2020), the ONC is doing what it can to publish its learnings on a monthly basis with resource documents.
The public is encouraged to connect with Posnack and the ONC in the following ways:
-
- Email: Steven.Posnack@hhs.gov
- Phone: 202-690-7151
- Health IT Feedback Form
- Twitter: @ONC_HealthIT
- LinkedIn: Office of the National Coordinator for Health Information Technology
- YouTube: Office of the National Coordinator for Health IT
Federal Programs Catalyzing Health Equity Initiatives

- Date: Tuesday, August 23, 2022
- Presenters:
- Larry Jessup, MHA, Branch Chief, Office of the National Coordinator for Health IT
- Sonia Chambers, Executive Director, West Virginia Health Information Network
- George Gooch, CEO, Texas Health Services Authority
- Denise Hines, DHA, PMP, FHIMSS, Chief Executive Officer, Georgia Health Information Network
- William Marella, MBA, MMI, Vice President, Value Based Care & Analytics, HealthShare Exchange
- Overview: HIE leaders from multiple states share information about their organizations’ participation and success in select federal programs.
In this session, HIE leaders from Pennsylvania and Delaware, Georgia, West Virginia, and Texas discussed their involvement in federal programs, with a focus on health equity.
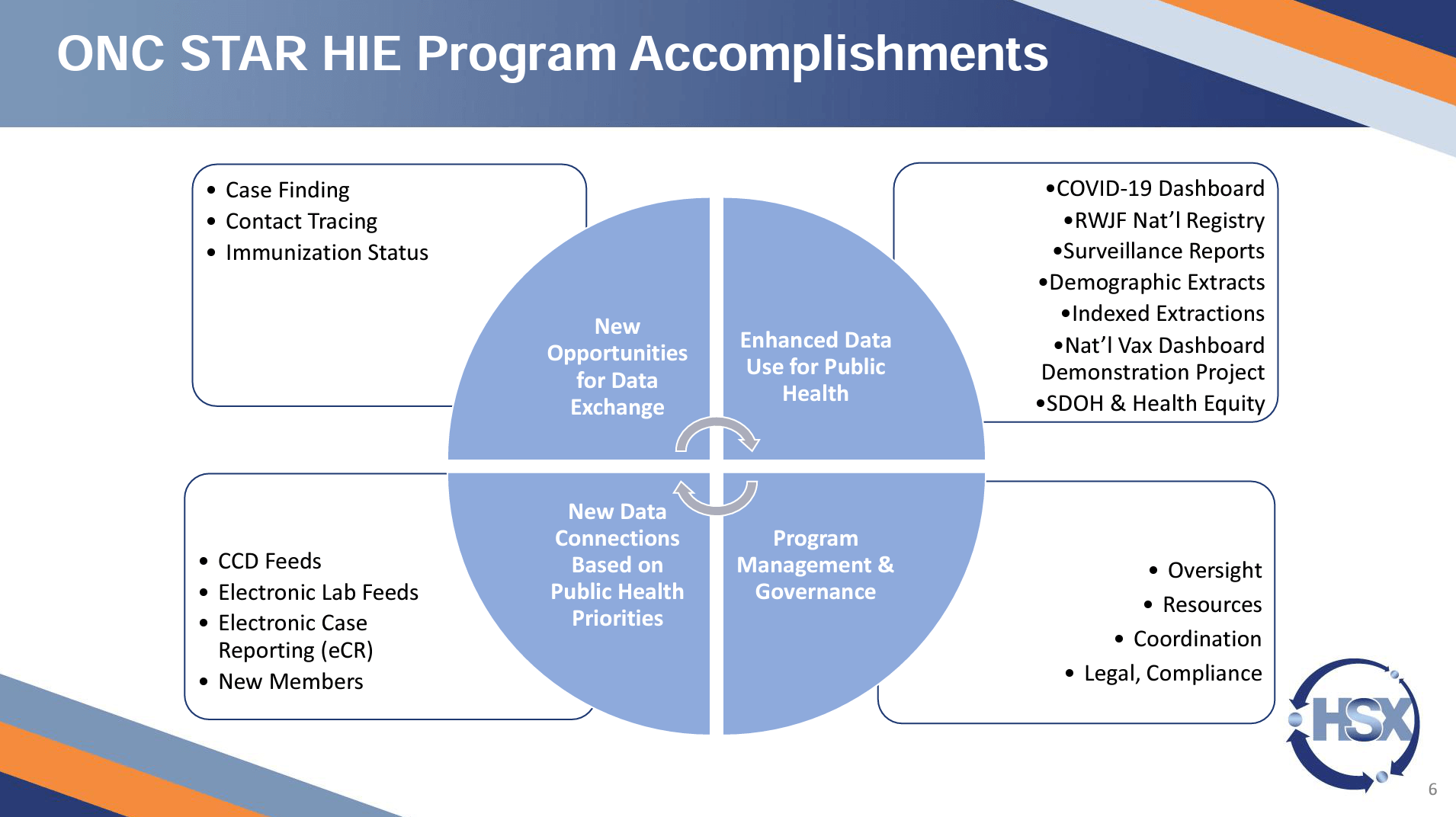
Such programs include the ONC’s Strengthening the Technical Advancement & Readiness of Public Health via Health Information Exchange (STAR HIE) grant program, which was designed to leverage health information made available by HIEs to support public health agencies, including for COVID-19 response efforts. The STAR HIE grant made available $5 million from the CARES Act (March 27, 2020) in two phases:
- $2.5 million to support five HIEs in creating services that benefit public health agencies.
- Supplemental $2.5 million to support 17 HIEs (including four of the original five recipients) to specifically support increased data sharing between immunization information systems (IIS) and HIEs.
The STAR HIE program seeks to build innovative health information exchange services that would benefit public health agencies and improve the health information exchange services intended to support communities disproportionately affected by the COVID-19 pandemic.
William Marella from HealthShare Exchange (HSX) described Delaware’s accomplishments as part of the STAR HIE program, including case finding, contract tracing, a COVID-19 dashboard, surveillance reports, demographic extracts, support for a national vaccination demonstration project, and advancing the prioritization of SDOH data and health equity efforts. The HIE provided specific value to COVID-19 response work by offering more up-to-date patient information than individual stakeholder organizations had in their own systems. HSX was able to send files with member vaccination status back to organizations and agencies to help them identify homebound patients in order to mobilize EMS or visiting nurses to go to people’s homes to provide vaccinations for those unable to get to vaccination locations.
As a result of their successes, HSX has been able to expand public health use cases, onboard county health clinics, and support medical examiners’ offices and mortality review committees with HIE data. HSX is also now involved in a new partnership with the Pennsylvania Department of Aging, connecting residents with 19 different benefit programs. The program has also implemented a closed-loop referral program in Pennsylvania.
The Georgia Health Information Network (GaHIN) is Georgia’s state-designated HIE and has over 25,000 connected providers. GaHIN is also connected to five state agencies, all of the Georgia Care Management Organizations, correctional facilities, and multiple public health registries (Alzheimer’s, Immunizations, eLabs, Birth Defects, and Cancer). GaHIN was the first organization of its kind in the country to partner with the American Heart Association on the AHA’s Get With the Guidelines(R) initiative as a technology partner for data submissions.

GaHIN was an early adopter of query-based exchange and currently supported over 10 million queries last year. Today, providers can send secure messages to patients in the public registries, and agencies can view information about children in their care. GaHIN’s STAR HIE grant facilitates the connection of clinical facilities associated with the Veterans Administration across Georgia, state correctional facilities, and hospitals that are not currently sending COVID-19 test results through the HIE.
The outreach team has contacted 32 hospitals to date, built five new connections (1 contributing COVID-19 data so far), and has advanced discussions and preparatory work with dozens of others. GaHIN has also partnered with HI-BRIDGE HIE to expand connected correctional facilities and transmit relevant data. Since 2021, HI-BRIDGE HIE has grown from four to thirteen correctional facility connections. Discussions are underway with more correctional facilities at this time.
The GaHIN team has created flat files from provider HL7 data to send to Medicaid for public health initiatives and to the Governor’s office to make executive decisions. GaHIN continues to participate in the ONC STAR HIE Health Equity Workgroup, originally a short-term initiative that has been continued due to demand among grant program participants. The workgroup is a forum for educational presentations on topics such as provider needs, advancing the use of SDOH data, health equity challenges, digital health equity, the Gravity Project, and expanding telehealth use at a public health level during the pandemic.
West Virginia Health Information Network (WVHIN) is the state-designated HIE in West Virginia. The HIE had connectivity with many organizations, technical know-how, and relationships in place at the state and local levels, but the state only had electronic lab reporting from four sources when COVID-19 began. The HIE worked to complete twenty new connections in about two weeks. As rapid tests started to be used in new locations (assisted living facilities, etc.), the state started mandating electronic reporting.
WVHIN partnered with CRISP to provide a lightweight form for people to fill out at alternate testing sites to improve electronic data collection and submission. West Virginia followed Maryland and Washington, D.C. by taking race and ethnicity from already available data and sending it to the state for planning and decision-making. In many cases, treating physicians did not know their patients tested positive. Because WVHIN was able to help supply essential data to the state, the state reciprocated by providing data that WVHIN used for general alerts and outreach to providers.
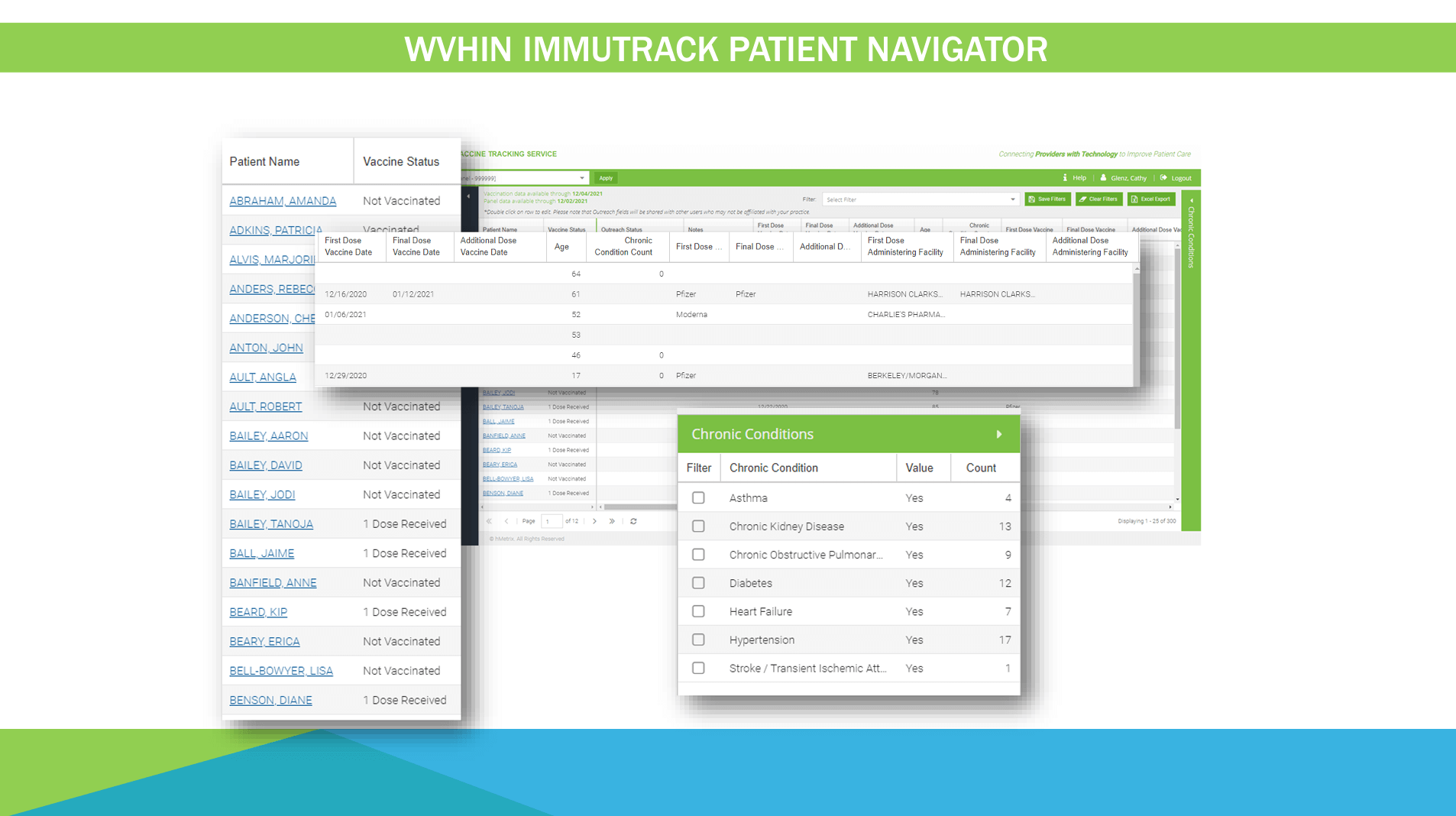 WVHIN also took difficult-to-match data and created new information products to notify care managers in Medicaid managed care organizations, FQHCs, and others to help them see which patients had been vaccinated. This data could be sorted by race, ethnicity, geography, or by chronic conditions. At an individual level, vaccine information shows where patients were vaccinated, the vaccine manufacturer, and folds in data about chronic conditions and claims data. Since the state does still have limited resources, marketing staff from the commerce department helped the effort by strategizing how best to use higher-level data and maps for outreach. These are examples of an HIE helping at both an individual level and simultaneously at a population health level.
WVHIN also took difficult-to-match data and created new information products to notify care managers in Medicaid managed care organizations, FQHCs, and others to help them see which patients had been vaccinated. This data could be sorted by race, ethnicity, geography, or by chronic conditions. At an individual level, vaccine information shows where patients were vaccinated, the vaccine manufacturer, and folds in data about chronic conditions and claims data. Since the state does still have limited resources, marketing staff from the commerce department helped the effort by strategizing how best to use higher-level data and maps for outreach. These are examples of an HIE helping at both an individual level and simultaneously at a population health level.
The STAR HIE program provided WVHIN with upfront funding for these efforts, but WVHIN has since been able to rely on their network for relationships to secure additional funding to continue their services, such as from the CDC. WVHIN is now part of the IDEAS collaborative and is working with IIS on data clean-up. WVHIN leadership feels that the organization is now well-positioned for other emerging opportunities and emergencies.
The Texas Health Services Authority (THSA) was one of the original five STAR HIE grant program awardees and was included in the supplemental award. THSA piloted a project to help over 600 hospitals in Texas transition from manually filling out spreadsheets containing situational awareness information (ventilators, bed capacity, etc.) to an automated and standardized process. THSA received their supplemental grant funding for a pilot with a rural critical access hospital related to vaccination data. Such rural stakeholders can often have challenges that other organizations do not. For instance, only having a single IT resource available to the facility to work on a variety of issues and projects one day per week.
THSA supports HIETexas, which customizes “smart alerts” to alert providers based on only certain diagnoses, admit reason text, source facilities, or other criteria. This approach to alerting can reduce alert fatigue for providers and release only the most relevant alerts for follow-up. Popular smart alerts include SDOH criteria based on ICD-10 codes and other indicators such as “experiencing homelessness.”
The presenters stated they appreciate federal agencies’ work to drive progress. They also encouraged forming new and creative relationships at the state and local levels.
Tackling Health Equity with Data Innovation and Partnerships
- Date: Tuesday, August 23, 2022
- Presenters:
- Erica Galvez, CEO, Manifest MedEx
- Abner Mason, Founder & CEO, SameSky Health
- Cheron Vail, Chief Information Officer, Health Plan of San Joaquin
- Lakshmi Dhanvanthari, MD, Chief Medical Officer, Health Plan of San Joaquin
- Overview: In this session, leaders from Manifest MedEx, the Health Plan of San Joaquin, and SameSky Health discuss their recent collaboration to customize outreach to patients and providers for significantly improved engagement and results.
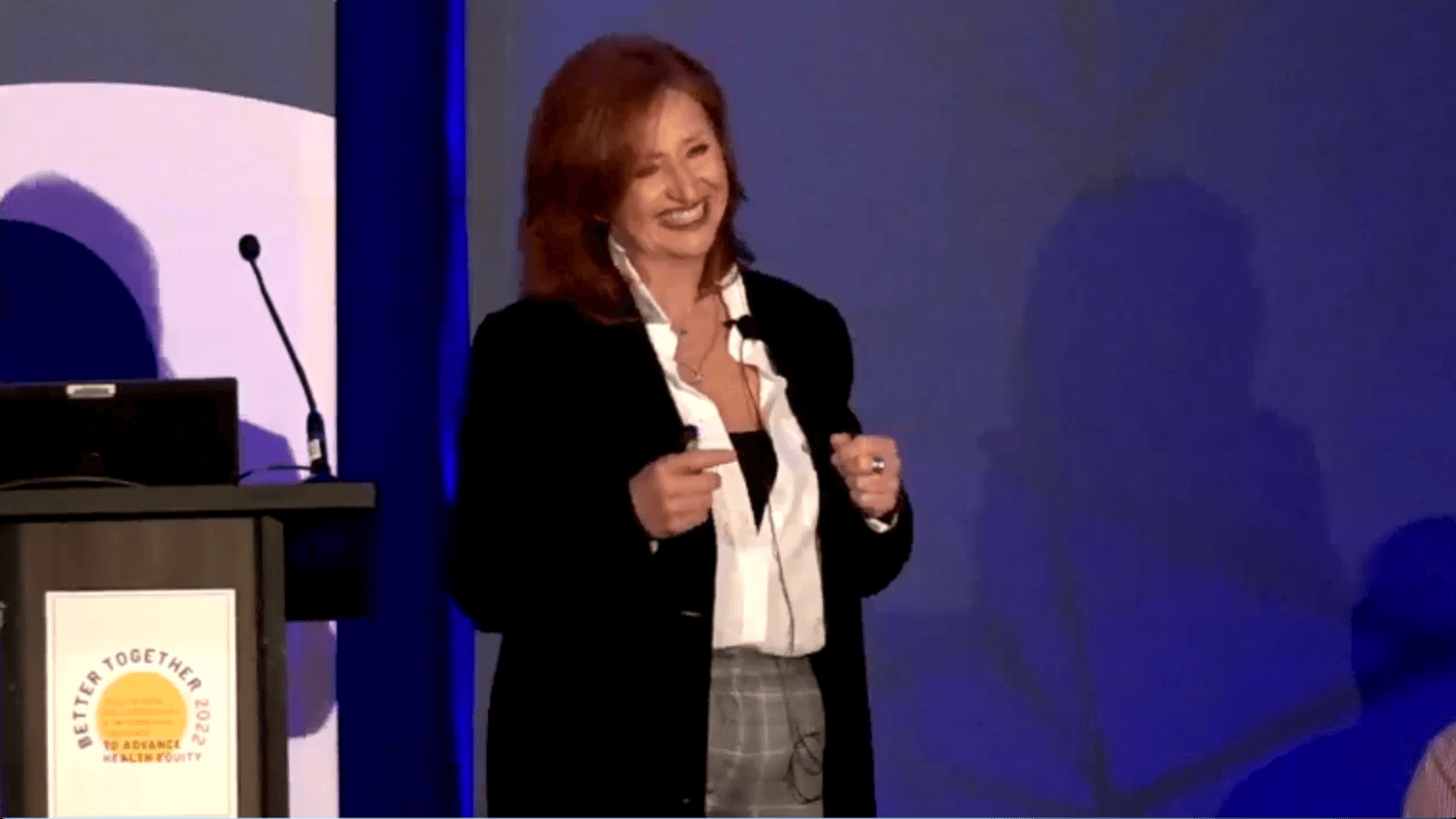
Manifest MedEx (MX) is the largest non-profit HIE in California, combining claims and clinical data into longitudinal records for about 30 million patients. MX’s CEO, Erica Galvez, opened the session by introducing today’s speakers and explaining that health equity continues to be a priority for MX and the state of California.
 The Health Plan of San Joaquin (HPSJ), also in California, serves as the local non-profit initiative and leading Medi-Cal managed care plan for San Joaquin and Stanislaus counties. Now over 25 years old, HPSJ coordinates care for over 400,000 members and connects those members to 345 primary care providers, over 3,100 specialists, and 11 plan network hospitals. HPSJ employs over 425 individuals and engages members, communities, and providers, making the health plan a vital link across sectors to address SDOH and optimize health equity for the people they serve.
The Health Plan of San Joaquin (HPSJ), also in California, serves as the local non-profit initiative and leading Medi-Cal managed care plan for San Joaquin and Stanislaus counties. Now over 25 years old, HPSJ coordinates care for over 400,000 members and connects those members to 345 primary care providers, over 3,100 specialists, and 11 plan network hospitals. HPSJ employs over 425 individuals and engages members, communities, and providers, making the health plan a vital link across sectors to address SDOH and optimize health equity for the people they serve.
Cheron Vail and Lakshmi Dhanvanthari shared some of the specifics about HPSJ’s outreach project. When COVID-19 emerged, HPSJ knew that they would need to engage their members and stakeholders to provide education and outreach. Managed Medi-Cal Health Plans were required to contact high-risk members to encourage them to get a COVID-19 vaccination. HPSJ needed to quickly determine which members were considered high-risk and devise an approach to perform the outreach. HPSJ needed to understand their member population based on age groupings and specific criteria, such as those who were homebound, living with comorbidities, and other criteria.
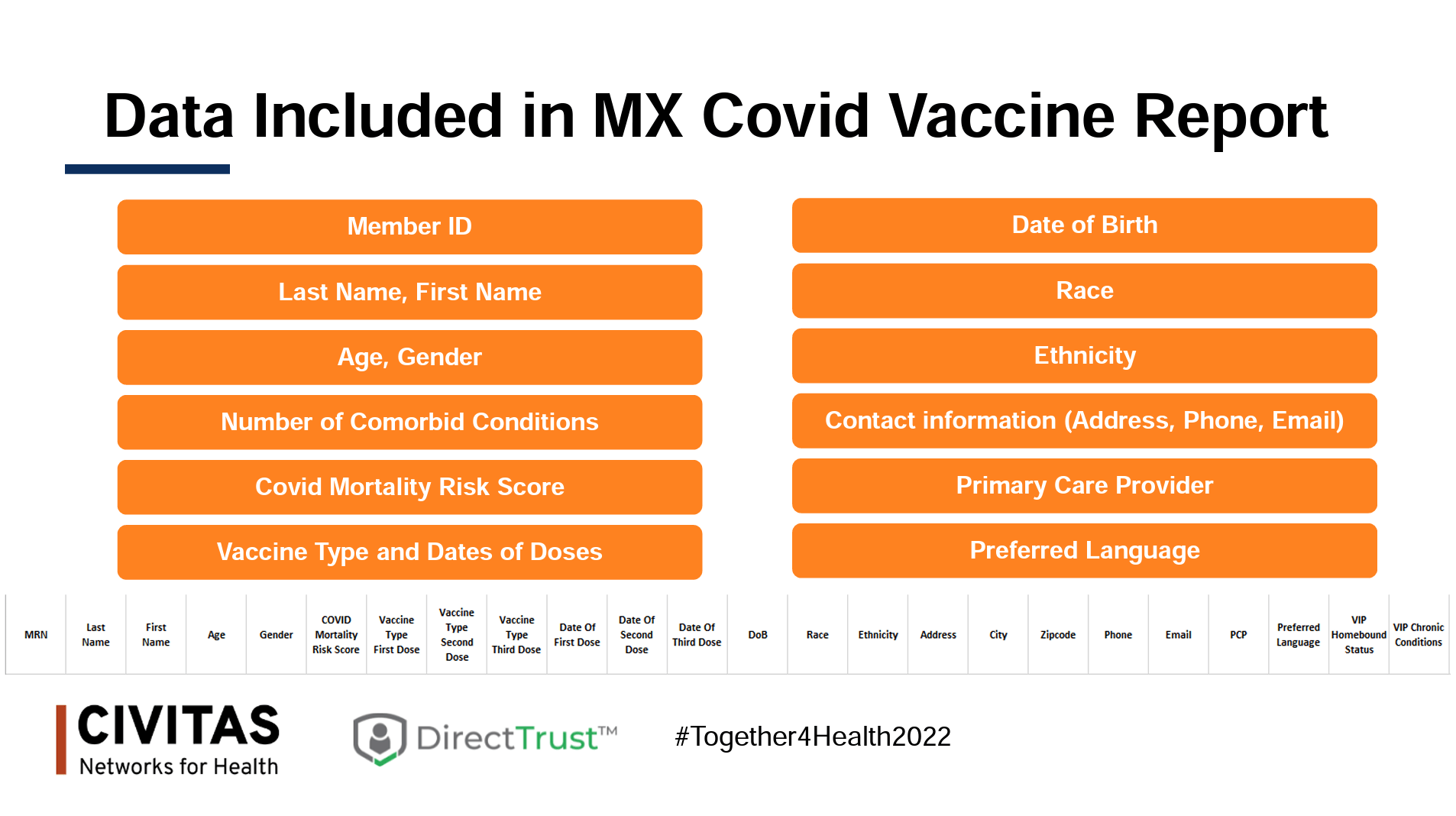 HPSJ was able to turn to MX to collaborate on these data and outreach needs. HIEs can complement a health plan’s IT department to supplement reports and data extracts, as well as link data from sources not directly available to the health plan. In this particular partnership, vaccine registry data files were shared with MX, who then joined this data to additional provider information, current member demographics (including race and ethnicity data from other sources), and COVID-19 risk scores. MX then returned a comprehensive and easy-to-sort aggregate file that allowed HPSJ to identify members meeting specific criteria, including whether they already had one or more vaccine doses. At-risk sub-populations were identified and provided to SameSky Health, which works with Medicaid managed care and Medicare plans to implement their personalized outreach services.
HPSJ was able to turn to MX to collaborate on these data and outreach needs. HIEs can complement a health plan’s IT department to supplement reports and data extracts, as well as link data from sources not directly available to the health plan. In this particular partnership, vaccine registry data files were shared with MX, who then joined this data to additional provider information, current member demographics (including race and ethnicity data from other sources), and COVID-19 risk scores. MX then returned a comprehensive and easy-to-sort aggregate file that allowed HPSJ to identify members meeting specific criteria, including whether they already had one or more vaccine doses. At-risk sub-populations were identified and provided to SameSky Health, which works with Medicaid managed care and Medicare plans to implement their personalized outreach services.
SameSky Health offers a technology platform that collects and aggregates public data and integrates cultural awareness planning and language customization to plan and carry out messaging campaigns that optimize patient interaction and trust. SameSky provides outreach services for health plan members on wellness, education, and safety topics. The company focuses on building trusted relationships that “encourage dignity, autonomy, and companionship as [health plan members] navigate disparate life experiences within a complex healthcare system.”
We tend to see one size fits all approaches to outreach, seemingly hoping that broad, singular messages will reach at least most of a given population. However, this approach ignores the importance of building trust and putting messages into words/engagement strategies that make people feel connected and willing to interact with the message sender. SameSky works to meet patients where they are and understand them at a deeper cultural level, enabling better care and more genuine relationships with care teams and health plans. In short, messages can and should feel personal if we expect to influence patients to do things they might not normally do (such as getting a vaccine).
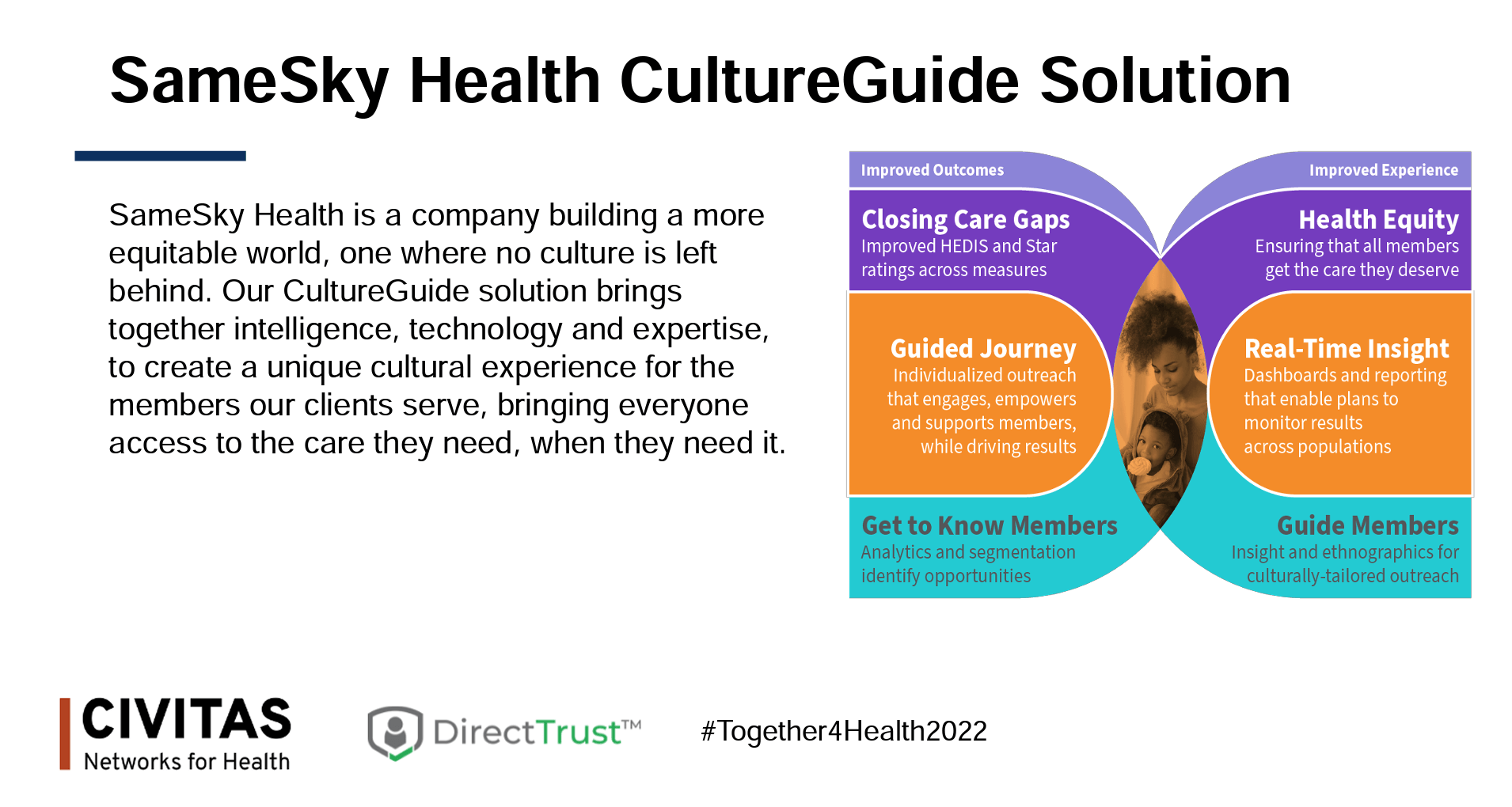 Insights from CultureGuide, SameSky’s health equity/ engagement solution, showed specific Spanish-speaking members who had transportation barriers, lived in multi-generational households where group vaccination efforts might be needed, and had experienced technical and literacy barriers. For these individuals, targeted communications with tailored language led to arranging group vaccinations as well as transportation for family members.
Insights from CultureGuide, SameSky’s health equity/ engagement solution, showed specific Spanish-speaking members who had transportation barriers, lived in multi-generational households where group vaccination efforts might be needed, and had experienced technical and literacy barriers. For these individuals, targeted communications with tailored language led to arranging group vaccinations as well as transportation for family members.
Abner Mason, SameSky’s founder and CEO, offered the following takeaways from their work so far:
- We must personalize engagement. Generic messaging won’t work.
- We must use data to personalize. Leverage available data about race, ethnicity, language preferences, cultural details, and other factors where possible. Using data in this way helps your organization to “meet them where they are” and build trust.
- Listen. Most outreach is one-way. It is important to avoid just talking “at” people. Text messaging is a key technology to reach patients wherever they are and in a way that they are more likely to respond and interact with you.
- Don’t judge. So much of the COVID-19 communication that Mason saw during the pandemic carried bias and judgment. We must emphasize showing humility and civility. As Mason put it, “we have to listen to all the craziness and build bridges to rational approaches.”
According to Dhanvanthari, HPSJ’s vaccination rate increased from 5% in March 2021 to 54% for patients twelve years old and older and 47% for patients five years old and older in July 2022. For homebound patients, HPSJ partnered with public health agencies to send nurses to patients’ homes to assist them with vaccinations. Reports and data continue to be used by stakeholders, and HPSJ is looking for more ways to improve care and services through HIE partnerships.
California has recently identified new quality metrics that health plans need to track. Vail provided the following example: When members show up in the ED with specific conditions, health plans need to ensure follow-up within 30 days with appropriate providers. Due to the delay in claims data, it might not always be possible to meet the 30-day requirement. HPSJ and MX discussed using ADTs to provide an alert in a more timely manner for members arriving at an ED with certain diagnoses or treatments. After the team determined which data elements were needed, data is now sent to HPSJ two to three times per week and given to HPSJ’s medical management department for follow-up with members. HPSJ then periodically reconciles the data with claims data to ensure accuracy. Partnerships such as this make it possible to take action earlier and directly affect patient outcomes.
 Mason added a few bonus takeaways from the outreach project. He stated that it is important to have mechanisms in place to learn from patient feedback. As part of the text message campaign, the SameSky team found points of confusion that negatively affected members’ ability to complete a vaccination appointment. Specifically, the text message campaign told members that vaccines were cost-free. However, when members showed up at a vaccination site, one of the first questions they were asked was whether or not they had insurance. Many were not prepared for this and assumed they were going to have to pay something. Some of them texted back to SameSky, saying that the vaccine was not free. The staff listened and investigated/altered their messaging to inform members how to navigate the questions that staff at vaccination sites might ask. In a similar way, undocumented people will leave when the first questions are insurance related. Messaging and access to services need to be friendlier.
Mason added a few bonus takeaways from the outreach project. He stated that it is important to have mechanisms in place to learn from patient feedback. As part of the text message campaign, the SameSky team found points of confusion that negatively affected members’ ability to complete a vaccination appointment. Specifically, the text message campaign told members that vaccines were cost-free. However, when members showed up at a vaccination site, one of the first questions they were asked was whether or not they had insurance. Many were not prepared for this and assumed they were going to have to pay something. Some of them texted back to SameSky, saying that the vaccine was not free. The staff listened and investigated/altered their messaging to inform members how to navigate the questions that staff at vaccination sites might ask. In a similar way, undocumented people will leave when the first questions are insurance related. Messaging and access to services need to be friendlier.
TEFCA: Dispelling Myths, Highlighting Motivations, and Understanding Participation
- Date: Tuesday, August 23, 2022
- Presenters:
- Alan Swenson, Executive Director, Carequality
- Julie Maas, MEng, MBA, Chief Executive Officer, EMR Direct
- Jay Nakashima, MBA, Executive Director, eHealth Exchange
- Steven Lane, MD, MPH, Clinical Informatics Director for Privacy, Information Security & Interoperability Sutter Health, Office of the National Coordinator for Health IT
- Lisa Bari, MBA, MPH, CEO, Civitas Networks for Health
- Jon Elwell, CEO, Kno2
- Zoe Barber, MPH, Policy Director, The Sequoia Project
- Overview: Lisa Bari, CEO of Civitas Networks for Health, leads a panel of TEFCA experts through a discussion on how companies and HIEs are evaluating their potential involvement in TEFCA and whether QHIN designation makes sense for them and their stakeholders. Sequoia Project policy director Zoe Barber then provides the latest on QHIN applications and the TEFCA timeline.
Zoe Barber, policy director at The Sequoia Project, began the session by addressing some common myths about TEFCA. As of January 2022, version 1 of the Common Agreement and QHIN technical framework were released. More than 10 Standard Operating Procedures (SOPs) are in varying stages of completion and are necessary to help improve clarity for those interacting with TEFCA. Look for more activity on SOPs in the near future.
 Barber explained that while many have heard announcements from organizations across the country declaring their interest in becoming QHINs, please know that a final application has not yet been published. Sequoia has been collecting feedback on drafts and released additional topics that the application might cover to solicit feedback. A final version should be available now (end of August), followed by a 30-day buffer period before applications will be accepted. Barber strongly encouraged potential applicants to use that buffer to carefully review requirements and processes.
Barber explained that while many have heard announcements from organizations across the country declaring their interest in becoming QHINs, please know that a final application has not yet been published. Sequoia has been collecting feedback on drafts and released additional topics that the application might cover to solicit feedback. A final version should be available now (end of August), followed by a 30-day buffer period before applications will be accepted. Barber strongly encouraged potential applicants to use that buffer to carefully review requirements and processes.
Following the application process, it will take some time to actually designate QHINs, and when that happens, it will be done in cohorts, not individually. The goal will be to build a critical mass of designated QHINs to establish a governing body.
Barber also wanted to make it clear that TEFCA will not “solve” interoperability. It will be critical infrastructure, but note that it is voluntary and is not meant to replace existing networks. Instead, it is meant to help accelerate connecting those existing networks across the country and drive alignment.
Becoming a designated QHIN is not going to be the right path for many organizations. CRISP, for example, has already signaled its intent to be a participant in a QHIN but not seek to become one on its own. QHIN designation will require considerable resources, and for most, it will not make sense for your business model. It might make more sense for organizations that already have similarly aligned processes and infrastructure. While participation is not mandatory, now is the time to think about how your organization is likely to fit in.
Organizers offer monthly information sessions and weekly “office hours” as opportunities to engage and provide feedback.
 Lisa Bari, CEO of Civitas Networks for Health, commented that what Barber described is what multi-stakeholder partnerships really look like. They often take a long time and should be thorough. Thoughts and processes evolve as people work through a complex process.
Lisa Bari, CEO of Civitas Networks for Health, commented that what Barber described is what multi-stakeholder partnerships really look like. They often take a long time and should be thorough. Thoughts and processes evolve as people work through a complex process.
Bari asked panelists to talk about their organizations’ interest in participating and plans for TEFCA.
Jon Elwell said that Kno2 is focused on interoperability, and they view TEFCA and QHINs as simply augmentation to their existing work, not a replacement or entirely different direction. Julie Maas from EMR Direct said that her organization provides identity and FHIR services for about 150 organizations. They do not yet have plans for participating as a QHIN but are reviewing the opportunities to see how they might fit. Generally, they also view TEFCA as augmenting current work and will look to their customers to indicate demand. Maas also noted that her company is very involved with HL7 FHIR events and, so far, they see TEFCA as following a lot of what was done with FHIR.
Alan Swenson is Executive Director of Carequality, which works with The Sequoia Project on the QHIN technical framework and roadmap. Swenson said that the QHIN framework models much of what has been proven successful through Carequality. In large part, the QHIN application, implementation guides, and SOPs follow existing Carequality models and documentation. Carequality sees over 350 million documents exchanged between networks each month, not including documents exchanged within networks. Swenson expects to see the current work, which has been focused on data exchange for treatment, expand significantly into non-treatment use cases (payment, operations, etc.). His hope is that government-sponsored initiatives like TEFCA will continue to drive us toward those new use cases.
 Today’s panel features special guest Steven Lane, MD, MPH. Dr. Lane has been involved in many aspects of national health data exchange and interoperability for many years. He has been a part of the Health Information Technology Advisory Committee (HITAC) since 2018, is a practicing family physician and informaticist, currently serves as chair of the board of The Sequoia Project, is chair of the Carequality Steering Committee, was co-chair of the DirectTrust Clinicians Steering Workgroup, and has been involved in a number of other workgroups, task forces, and professional organizations supporting their efforts to advance health IT. Dr. Lane was one of the first physicians to exchange across Carequality and will soon be joining Health Gorilla as their CMO. Health Gorilla aspires to be among the first QHINs.
Today’s panel features special guest Steven Lane, MD, MPH. Dr. Lane has been involved in many aspects of national health data exchange and interoperability for many years. He has been a part of the Health Information Technology Advisory Committee (HITAC) since 2018, is a practicing family physician and informaticist, currently serves as chair of the board of The Sequoia Project, is chair of the Carequality Steering Committee, was co-chair of the DirectTrust Clinicians Steering Workgroup, and has been involved in a number of other workgroups, task forces, and professional organizations supporting their efforts to advance health IT. Dr. Lane was one of the first physicians to exchange across Carequality and will soon be joining Health Gorilla as their CMO. Health Gorilla aspires to be among the first QHINs.
Jay Nakashima is the Executive Director of eHealth Exchange (eHX), which exists to expand state and regional HIEs’ reach beyond their existing boundaries. A few HIEs have already indicated their interest in joining TEFCA under eHealth Exchange if it becomes a designated QHIN. eHX plans to offer QHIN connectivity to its members as an included benefit, requiring no additional paperwork or extra steps.
Bari asked the panel about the pros and cons of applying to become a QHIN.
Maas explained that her company’s customers have the foundational interoperability that they want. However, as things evolve, if their customers begin to ask for QHIN connectivity, EHR Direct will respond to market demand. The company has a number of components in place (e.g., EHNAC accreditation) to position the company for QHIN involvement, but they are not yet ready to commit to making an application.
Elwell echoed this response and said that Kno2 is watching for market demand.
Nakashima said that eHX is looking at two drivers: The first includes signals from the federal government about whether there are going to be incentives or requirements. CMS is already encouraging TEFCA participation through the MIPPS program, which they see as a strong indication that participation could be required at some point in the future. The second item to consider is the promise of new use cases. Treatment-based exchange is well underway now (as of the last 1-2 years), but we have minimal activity today for payment solutions, individual access, authorizations, and public health. He is hopeful that the credibility of government backing will help to advance non-treatment use cases.
Bari then asked the panel about how they would rate our progress so far.
Dr. Lane responded by saying that we have a strong interoperability infrastructure today and a lot of data flowing where it was not before. The problem, however, is that it can be too much in some cases and, even more critically, is fragmented. The original plan for TEFCA was to provide a single on-ramp, which is attractive to providers. This is the real promise of TEFCA for a lot of people – simplifying the experience of connecting. TEFCA will not be perfect in the immediate future, but having a federally-backed solution to allow us to interact more seamlessly is valuable. Bari added that we need to continue the work at local and state levels to collect, move, and improve data in expanding Health Data Utility roles in order for that single on-ramp to have optimal value.
Bari commented that a lot of work has gone into Carequality and asked what its future might be.
Swenson said that Carequality will continue its work for now. It is too soon to determine whether Carequality will somehow be absorbed into TEFCA administration or remain independent. For at least the near term, organizations are likely to want to continue exchanging for treatment purposes through Carequality. Those not connected to Carequality could choose connectivity through TEFCA. We should also see new use cases emerging over the next few years, and those use cases will help to inform a trajectory.
The panel discussed individual access, i.e., patients getting access to their own data. Panelists generally felt that (1) there is a lot of work to do to handle individual access well, and (2) patient matching is both essential to individual access and perhaps the most difficult issue to solve. FHIR at scale efforts could provide a way forward in aggregating different matching models. Yet, while FAST could help with patient credentials, not all patients have usable credentials. Demographics-based matching might still be necessary alongside more sophisticated solutions. We will need to continue to work on this as a community of innovators to find other means of validating who people say they are. Panelists suggested looking to the FHIR Roadmap for TEFCA for guidance.
As the session ended, Bari encouraged attendees to meet the panelists at lunch. For those interested in meeting, here were some topics that panelists welcomed as discussion material:
- Jay Namashima: How the FDA retrieves data about adverse events from vaccines through eHealth Exchange by retrieving FHIR R4 exclusively
- Zoe Barber: TEFCA, QHIN applications, SOPs, and if you meet her in person, ask about her personal journey with healthcare and why all of this work is so meaningful
- Steven Lane: USCDI, information blocking, and transition to all electronic health information (EHI) access
- Alan Swensson: TEFCA, Carequality’s work, how to use what we already have in place today
- Julie Maas: FHIR at scale taskforce (FAST), Unified Data Access Profiles, and TEFCA FHIR Roadmap
Education and Communication as a Catalyst for Technology Adoption

- Date: Tuesday, August 23, 2022
- Presenters:
- Katherine Lusk, Vice President Strategic Partnerships, Texas Health Services Authority
- Liz Buckle, Director of Product, CommonWell Health Alliance
- Kristian Feterik, MD, MBA, ABPM-CI, Medical Director, Interoperability, UPMC
- Anne Santifer, Director, Arkansas Department of Health – SHARE
- Kathryn Ayers Wickenhauser, MBA, CHPC, CHTS, Director of Communications, DirectTrust
- Overview: Representatives from the Texas Health Services Authority, CommonWell, UPMC, Arkansas SHARE, and DirectTrust discuss the importance and hallmarks of intentional, simplified, and engaging communication in today’s market.
Technology is no longer the main barrier to interoperability. What we are seeing today, instead, is that people do not always understand how to use available technology to most efficiently connect multiple types of data and systems. Of course, we still have opportunities to improve data quality and definitions or standards, but we are past the point of blaming technology for hindrances.
The panelists believe that, ultimately, our biggest challenges today stem from how we communicate our stories and whether or not we communicate well enough to bring everyone to the same level of understanding. We must focus and refine our ability to explain why a given technology or piece of data matters to the audience.
 We might realize, for example, that how a person speaks varies depending on whom they are speaking to. Or, we might over-communicate “noise,” in the recipient’s opinion, such as in the case of alert fatigue among providers. If providers are not given the right information and context to understand how they should use that information, then it leads to frustration and avoidance, meaning that we fail at our promise of effectively leveraging the technology that is available to us. In the case of providers, we really have to think about how our message fits into workflows.
We might realize, for example, that how a person speaks varies depending on whom they are speaking to. Or, we might over-communicate “noise,” in the recipient’s opinion, such as in the case of alert fatigue among providers. If providers are not given the right information and context to understand how they should use that information, then it leads to frustration and avoidance, meaning that we fail at our promise of effectively leveraging the technology that is available to us. In the case of providers, we really have to think about how our message fits into workflows.
 The Texas Health Services Authority (THSA) facilitates the Texas Interoperability Collaborative, a “multidisciplinary, vendor agnostic collaborative serving the state of Texas with improved care delivery, streamlining of administrative processes, and cost control through trusted cooperation.” Stakeholders bring work projects, and their priorities are central to the collaborative. The group meets on the second Wednesday of every month at 8 AM Central. Meetings are open to everyone.
The Texas Health Services Authority (THSA) facilitates the Texas Interoperability Collaborative, a “multidisciplinary, vendor agnostic collaborative serving the state of Texas with improved care delivery, streamlining of administrative processes, and cost control through trusted cooperation.” Stakeholders bring work projects, and their priorities are central to the collaborative. The group meets on the second Wednesday of every month at 8 AM Central. Meetings are open to everyone.
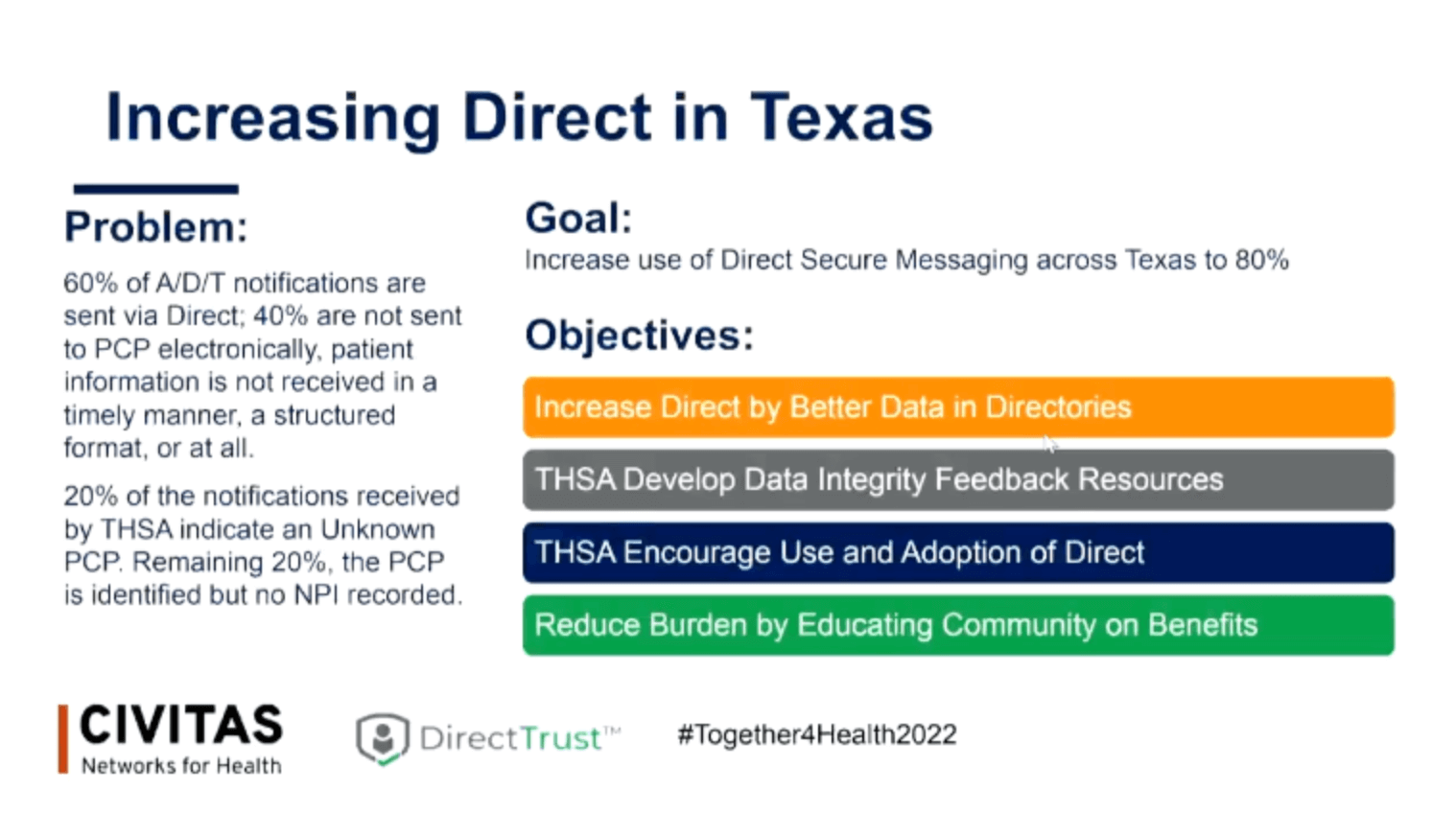
One of the focus areas is increasing Direct Secure Messaging across the state. HIE participation fees can be prohibitive for some entities, but Direct is a standard with wide enough appeal and accessibility that barriers to participation are thought to be low. In addition to increasing adoption across Texas, the collaborative is working to provide more context for Direct messages and improve the completeness of information associated with messages. The goal is to simplify communications and workflows. This goal, however, requires consistent core data to make messages effective. For example, an estimated 60% of ADT notifications are sent via Direct, but 20% of the notifications received by THSA indicate an “unknown” PCP. In other instances, the PCP is identified, but no NPI is available.
As a result of these challenges, the Texas collaborative’s goal is to increase the use of Direct Secure Messaging across the state to 80%. This process will be done by increasing Direct with better data in directories, developing data integrity feedback resources, encouraging the use and adoption of Direct, and reducing any burden by educating the community about the benefits of using this standard. Some communication efforts include simple tactics like updating fax cover sheets that ask recipients to consider using Direct Secure Messaging. THSA is also promoting a CCDA tool developed by Sarokar Deep that allows users to measure outbound documents and summarize/measure what data is included in documents. Other examples include placing stickers on fax machines reminding users to consider conducting a Direct address search prior to faxing.
The Arkansas State Health Alliance for Records Exchange (SHARE) is a state-wide health information exchange and offers an example of investing in improved communication. SHARE hired a recent college graduate and made her their social media specialist. At the time, SHARE did not have a strong promotion program. They used social media to tag clinics, reshare posts, and publish a quarterly newsletter that SHARE leaders felt was very simple and light.
CommonWell provides a different take on communication and education. Years ago, CommonWell’s focus was on technology. Today, the organization thinks more about partnering and educating multiple audiences. Education efforts feature storytelling and engaging visualization.
One suggestion from the panel is to save files or images from other organizations when you see examples of stories that are told in simple and effective ways that make sense. You can adapt these for your own organization to help improve the effectiveness of your communications.
 Part of THSA’s success in communicating and engaging the community is to ask the collaborative’s members to commit to taking what they learn and communicating it to their respective communities. Everyone is held directly accountable for moving information and insights and not passively attending meetings and events.
Part of THSA’s success in communicating and engaging the community is to ask the collaborative’s members to commit to taking what they learn and communicating it to their respective communities. Everyone is held directly accountable for moving information and insights and not passively attending meetings and events.
Your organization might also consider adding attending provider information to reports for rural providers. This added information gives them a quick and accessible way to call and immediately speak with the attending provider while the patient is still in the hospital and participate in influencing the patient’s care by providing additional information or context for the attending provider.
 At UPMC, leadership is looking for ways to engage medical students to learn more about informatics so that clinical decision support tools do not just come across as seemingly unhelpful alerts. Instead, medical students are educated about the HEDIS measure that might appear in a given alert and provided with the necessary context to understand and put the alert to use.
At UPMC, leadership is looking for ways to engage medical students to learn more about informatics so that clinical decision support tools do not just come across as seemingly unhelpful alerts. Instead, medical students are educated about the HEDIS measure that might appear in a given alert and provided with the necessary context to understand and put the alert to use.
Panelists discussed the need to extend partnership-building efforts and to listen to stakeholders more intently. You likely have the technology to solve their problems, but it’s critical to understand, be understood, and align. We now need to find new ways to bridge the gaps between potentially dense or fragmented data and the stories that the data need to convey.
The session moved to a Q&A period. One attendee asked about listening and, specifically, where listening occurs for the panelists. Examples include medical leadership committees or similar forums where providers feel comfortable expressing their feelings, user groups representing hospitals and providers, nurse informatics councils, or take low adoption of a service or solution as silent feedback about something that needs to change. If you struggle finding groups or opportunities like this, think about creating your own work groups. Many stakeholders, including providers, are often willing to participate.
One panelist added that sometimes how a person dresses or speaks can be an important part of aligning messaging to a given audience. They gave the example of needing to be aware that wearing a suit to a rural medical practice might lead to resistance to hearing your message. In some cases, you might need to think about dressing or looking more like your audience to improve receptivity to the story you want to tell (e.g., jeans and a polo shirt instead of a suit).
In general, panelists expressed the need to start with simple stories and then introduce the technology and data that support the story later. For example, show how workflows can be simplified and made more efficient. Then, after you have some level of engagement and interest in the time savings or other demonstrated value, explain the technology or solution that leads to the value you gave while telling your story.
Aligning your communication with your intended audience is essential to finding common ground, establishing new partnerships, building relationships, and enhancing buy-in and accountability. HIEs today are investing in the people and skills necessary to deliver high-impact messaging that is engaging, personalized, and convincing.
Lessons from California: Public-Private Collaborations to Foster Data Exchange

- Date: Tuesday, August 23, 2022
- Presenters:
- Timi Leslie, President, BluePath Health
- John Ohanian, Director, Chief Data Officer, Center for Data Insights and Innovation, California Health and Human Services Agency
- Lori Hack, MBA, CEO, California Association of HIEs (CAHIE)
- Katie Heidorn, MPA, Executive Director, Insure the Uninsured Project
- Overview: Leaders from Connecting for Better Health, the California Center for Data Insights and Innovation, the California Association of HIEs, and the Insure the Uninsured Project discuss the importance of bringing new voices into discussions about data exchange, strong leadership and commitment at the state level to support information sharing, and the value of California’s Data Exchange Framework in jumpstarting productive collaborations across the state.
The session was led by Timi Leslie, director of Connecting for Better Health. Lori Hack from the California Association of HIEs (CAHIE) opened the session with a presentation to set the stage for the upcoming facilitated discussion.
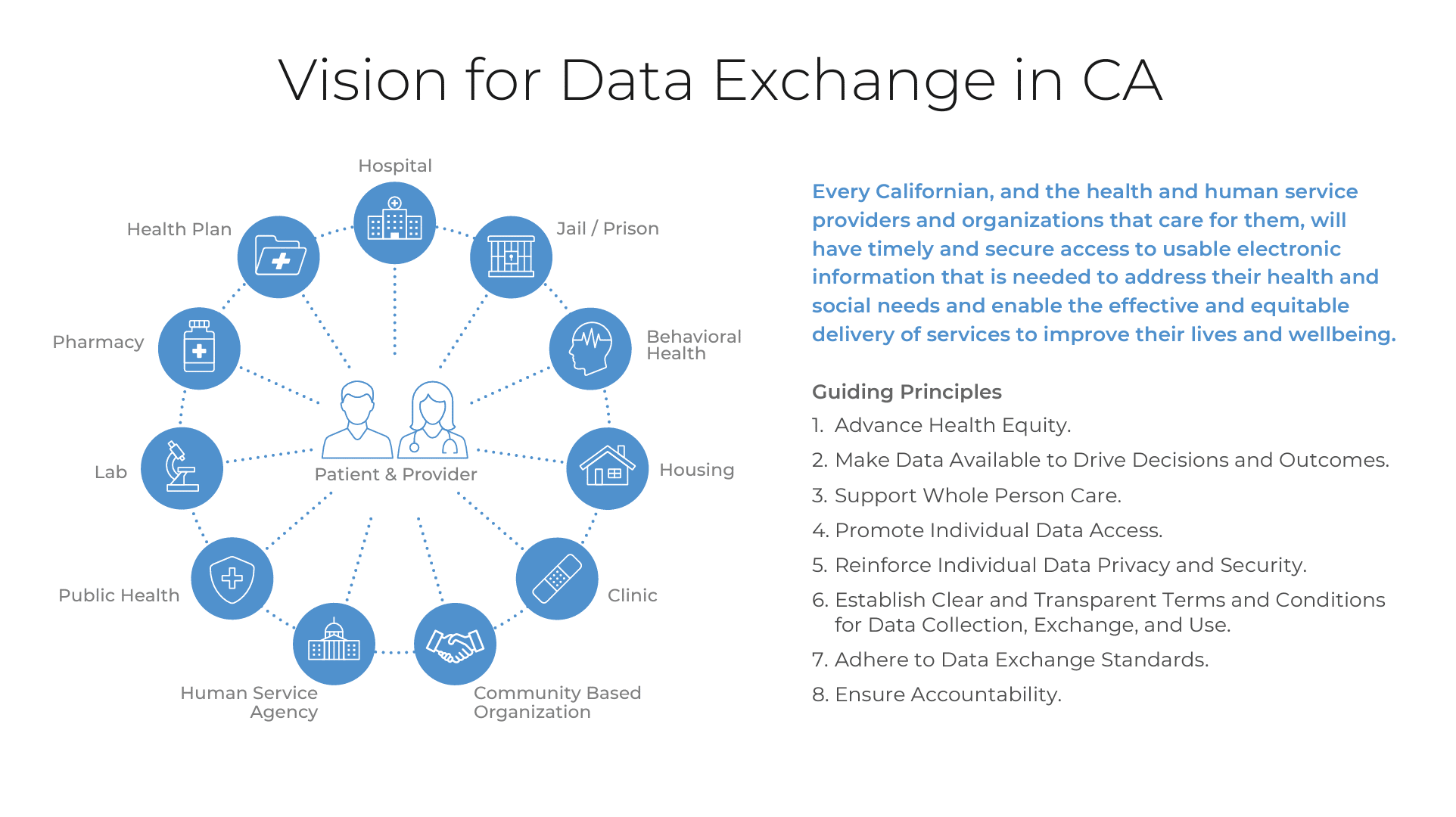
About a year ago, the state of California passed a mandate that facilitates data exchange, known as Data Exchange Frameworkt. The framework is based on the following guiding principles:
- Advance health equity
- Make data available to drive decisions and outcomes
- Support whole person care
- Promote individual data access
- Reinforce individual data privacy and security
- Establish clear and transparent terms and conditions for data collection, exchange, and use
- Adhere to data exchange standards
- Ensure accountability
 As others have shared at this conference, COVID-19 was an important accelerator and elevated inequities in our communities. While some in California feel that they lag behind other states in data exchange connections, success with this mandate shows significant progress in aligning ideas and priorities on topics like health equity and the use of health data for the public good.
As others have shared at this conference, COVID-19 was an important accelerator and elevated inequities in our communities. While some in California feel that they lag behind other states in data exchange connections, success with this mandate shows significant progress in aligning ideas and priorities on topics like health equity and the use of health data for the public good.
The state plans to follow the mandate with the following supportive actions:
- Governance: Establish CalHHS Data Exchange Board
- Participation: Energize mandated and non-mandated organizations to sign the Data Sharing Agreement
- Policies and Procedures: Publish additional policies and procedures to define who shares data and how
- Qualification: Create a process for qualifying health information organizations to share data on behalf of participants
- Identity and Consent: Implement the CalHHS Strategy for Digital Identities
Having a data-sharing agreement is expected to hasten and simplify participation across the state. Organizations will sign on over the next twelve months. As one might imagine, the process of getting to this point involved a lot of public and private conversations. An advisory board was established and included about 25 leaders from a range of organizations. Bringing more people to the table not only provided insight and input from stakeholders who might otherwise not contribute ideas, but it allowed members to educate others who were less aware of the data sharing already taking place across the state, as well as where data was being shared and where it was not.
The Insure the Uninsured Project (ITUP) is involved in consumer education and advocacy. Their charge is to bring people together. ITUP organizes a conference for state Medicaid stakeholders and hosts regional workshops. Their aim is to bring together local delivery systems, counties, and other government agencies. One of the most significant takeaways from their work to date is the need for growth and sophistication in telehealth services, which also means connectivity and data exchange.
The public sometimes thinks of health-related organizations as being in the same space and working together, but in reality, organizations work differently and have different, sometimes competing, financial incentives and priorities. Given these fundamental differences, it is remarkable that California now has a mandate that requires collaboration between these types of organizations.
 John Ohanian specifically credited Undersecretary Marko Mijic for bringing this together. Ohanian said that these kinds of efforts are not technology problems but leadership problems. Progress on challenging topics like this, where impasse is frequent, comes from strong leadership at the top.
John Ohanian specifically credited Undersecretary Marko Mijic for bringing this together. Ohanian said that these kinds of efforts are not technology problems but leadership problems. Progress on challenging topics like this, where impasse is frequent, comes from strong leadership at the top.
While there are many conversations underway at the state level to determine specific priorities, there is a general movement now to focus on person-centered approaches to delivering solutions. Having a technical framework is the first step. In parallel, California is planning to offer grants to encourage and support change.
California’s Center for Data Insights and Innovation (CDII) is offering $50 million in grants to help with onboarding and connectivity. The Department of Human Services also announced $200 million in grant funding for practice transformation to help connect to information-sharing networks and move offices from paper to digital. Attendees can look for information webinars starting as early as September. The Department of Human Services is also working on building and improving its internal infrastructure to better see and serve the whole person.
Lori Hack from the California Association of HIEs talked about new conversations that are emerging as new funding vehicles from the state are announced. One such conversation occurred on the topic of the Behavioral Health Quality Improvement Initiative. Hack had an ad hoc discussion in the middle of a coalition presentation with the county behavioral health directors association about what specific milestones meant and how to engage HIEs to help them meet requirements. In many cases, funding is tied to health information exchange.
Katie Hiedorn from ITUP talked about how her organization is effectively stress-testing the Data Exchange Framework. The organization seeks to bring together different groups to focus on three major use cases: housing/homelessness, aging, and Women, Infants, and Youths (WIC). Hiedorn explained that everyone seemed very excited about these opportunities, and the conversations were encouraging and showed pride in efforts to work on data sharing between these kinds of services. A lot of this excitement has to do with having a framework to initiate and align conversations.
 Within the next year, CDII expects to create a governing board and an advisory committee. Now that the framework is available, the state needs to work quickly to build the support necessary to make all of this work for the long haul as they work toward additional legislation. In the meantime, there will be committees working on refining policies and procedures internally, in addition to a process to qualify HIOs for the state and select areas of focus for the coming years.
Within the next year, CDII expects to create a governing board and an advisory committee. Now that the framework is available, the state needs to work quickly to build the support necessary to make all of this work for the long haul as they work toward additional legislation. In the meantime, there will be committees working on refining policies and procedures internally, in addition to a process to qualify HIOs for the state and select areas of focus for the coming years.
According to Hack, there has been a critical shift from the heavy lifting of bootstrapping information exchange efforts to much more fluid and productive discussions happening now due to state-level leadership.
Hiedorn added that efforts have been start-and-stop since the 1990s. Now, with a mandate and specific framework in place as a rallying point, there is a new level of excitement and momentum to build the kinds of solutions that have been waiting for the opportunity to materialize.
Ohanian reminded the audience that despite this progress in California, there is still a lot to learn from other states. Infrastructure in government is not typically set up for minute-by-minute public health. It’s no longer a question of whether we should operate this way going forward. We simply need to. We need to keep the excitement while we get to work.
The panelists responded to a few questions from attendees. One of the major themes of the Q&A session was to get involved and start or add yourself to conversations. Call your state. Participate in committees and community conversations. It is important not to wait. Many people in less explored niches are willing to talk and share valuable information. For example, WIC in California is very excited about data sharing because they are partly a social services organization, but there is a medical component. There are many other similar examples of places where new data-sharing opportunities are emerging and can really add value to the work HIEs are doing. As a general piece of advice, do not stop or slow down your organization’s storytelling and bridge-building efforts, as this is the time to find those new linkages and take advantage of the momentum.
Learning from Our Past: Improving Health Equity through Proactive Standards, Interoperability and Cross Sector Governance
- Date: Tuesday, August 23, 2022
- Presenters:
- Lisa Nicolaou, Cross Sector Data Sharing Program Director, MiHIN
- Mike Klinkman, MD, Professor, Department of Family Medicine, and Department of Learning Health Sciences, Briarwood Family Medicine/ University of Michigan School of Medicine
- Jaffer Traish, COO, findhelp
- Evelyn Gallego, MBA, MPH, CPHIMS, CEO, EMI Advisors
- Brian Handspicker, CTO, Open City Labs, Vestige
- Overview: Lisa Nicolaou, MiHIN’s SDOH Program Director, hosts a panel of experts from the University of Michigan School of Medicine, findhelp.org, EMI Advisors, and Open City Labs to review some of the pain points that have become today’s most pressing barriers in overcoming the pursuit of useful and free-flowing data between medical professionals and community based organizations.
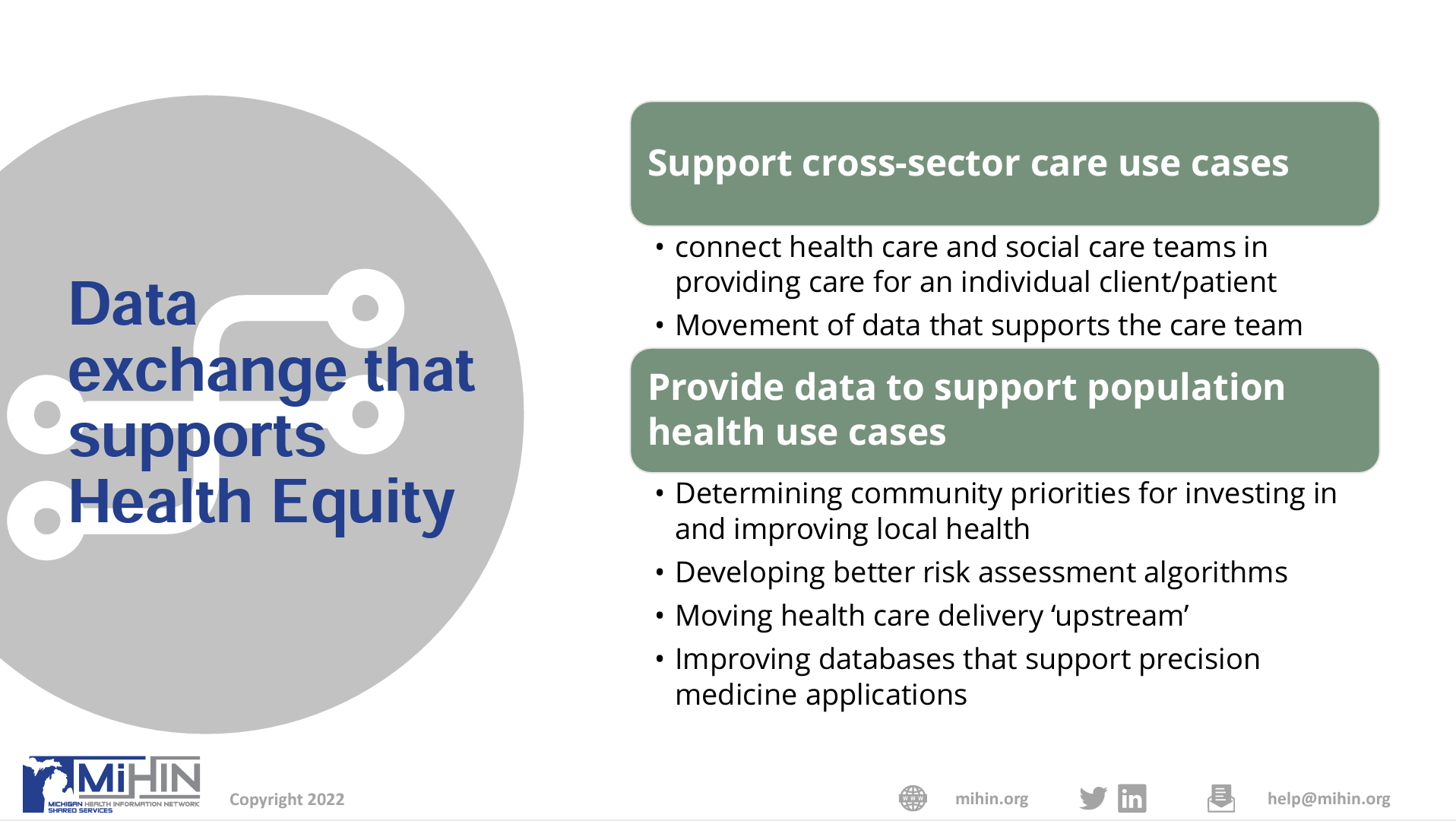
 Lisa Nicolaou, SDOH Program Director for the Michigan Health Information Network (MiHIN), opened the session with introductions and a brief overview of the current state of cross-sector data exchange (i.e., data from community sources beyond the traditional medical community). According to Nicolaou, there is extreme variability in approaches to improving cross-sector data. She cited examples, including San Diego-211 CIE, St. Louis RDA, and NCCARE360. There is limited “investment capital” for this realm of data, solutions tend to be vendor- or niche-driven, there is tension between OSFA and scalability, standards are still not fully adopted, and many efforts are “stuck,” perhaps due to funding or prioritization challenges.
Lisa Nicolaou, SDOH Program Director for the Michigan Health Information Network (MiHIN), opened the session with introductions and a brief overview of the current state of cross-sector data exchange (i.e., data from community sources beyond the traditional medical community). According to Nicolaou, there is extreme variability in approaches to improving cross-sector data. She cited examples, including San Diego-211 CIE, St. Louis RDA, and NCCARE360. There is limited “investment capital” for this realm of data, solutions tend to be vendor- or niche-driven, there is tension between OSFA and scalability, standards are still not fully adopted, and many efforts are “stuck,” perhaps due to funding or prioritization challenges.
In Michigan, progress is certainly being made, but Nicolaou noted that the HIE is now working to resolve issues that stem from governance not being in place in the past. Further, data platforms across the state vary widely. Some organizations use homegrown technology. Others are on robust platforms, but their data is also much more complex, such as in Detroit.
 Fortunately, payers in the state are reimbursing for social needs screenings in order to start to get data flowing, but the fundamental definition and collection challenges need to be solved to get the most value from new data. On a positive note, there has been an exponential increase in awareness about all of these issues, and change is happening.
Fortunately, payers in the state are reimbursing for social needs screenings in order to start to get data flowing, but the fundamental definition and collection challenges need to be solved to get the most value from new data. On a positive note, there has been an exponential increase in awareness about all of these issues, and change is happening.
MiHIN’s experiences show us a few things:
- Medical care culture is not the same as social care culture; goals for healthcare are not the same as goals for social care.
- Multi-sector alignment is extremely challenging; the speed of business, government, and community are all different.
- Assemblages are not the same as partnerships; simply bringing people into a room does not address power and money differences that affect commitments and decision-making.
- Knowing what data is needed to affect health equity requires research and evaluation, but this can be difficult to conduct, and there are questions about who pays for it.
- Community Based Organizations (CBOs) can be unique and different enough to not easily align on the same idea or incentive.
Nicolaou led today’s panel through a series of questions that sought to:
- Provide a baseline overview of the current cross-sector data exchange ecosystem nationally and in Michigan
- Identify the primary challenges to obtaining and exchanging health equity data
- Establish a role for HIE vendor-neutral approaches to working with social care platforms
- Outline opportunities and best practices that can create sustainable and scalable future cross-sector demonstrations
Question 1: What are the biggest challenges you see to moving data across sectors for the purpose of Health Equity?
Panelists offered a variety of thoughts, including policy and standards for consumer-direct consent, misaligned incentives, friction created by conflicting policies within and across levels of government, workflow design, mitigating legal liability for providers and organizations in this space, and extending the work done on frameworks for trust in the medical and HIE communities to social care frameworks.
Question 2: Is the urgency to better understand how unmet social needs impact health care outcomes, partially driven by the experience of COVID-19, a help or hindrance?
Responses showed mixed opinions. The urgency created by COVID-19 has accelerated awareness, funding, and relationship-building but has also perpetuated tactics to respond to requests and mandates as just another opportunity to “check the box” and move on. We’re still lacking underlying philosophical changes in some organizations, and the incentives are designed around dollars, which can cause us to miss what’s most important to focus on. Efforts often revolve around maximizing financial outcomes, not true health equity. Overall, panelists felt that the urgency has been more of a help than a hindrance.
Question 3: Healthcare learned that financial data alone is insufficient to improve quality. How does the healthcare experience in capturing data about care processes and care outcomes in a standardized manner relate to the work ahead in being able to capture and reuse data that documents social care delivery and cross-sector care coordination?
Some organizations are still focused on sharing only what they must share, not necessarily looking at what is being used and what is leading to better outcomes. We are putting a lot of information into EHRs and other repositories, but in many cases, we put the data in and then move on to something else and treat the collection of the data as just another administrative burden. If we use this approach to just whole-person results, we miss something. We need to align how we capture data with how we want it to be used to make a difference.
Question 4: Many organizations are focused on the problem of obtaining and exchanging data across the health and human services landscape. How do all of these organizations collaborate to move forward? What have we learned from our past to better inform movement going forward?
We really need to refocus ourselves on making the best use of standards. We’re creating a lot of them, but now we really need to converge efforts and agree on using them to get the results we want. There are multiple ways of handling things like directories. We now have efforts underway to attempt alignment, but separate models exist and create discrepancies. Maybe we need to agree on having a single directory for different kinds of information and consolidate our methods and tools for making referrals.
Question 5: How is social care workflow different from, or similar to, the healthcare workflow?
Community organizations work around understanding whole persons and their lives beyond disease. Medical settings work on problems. These differences lead to the disconnects that we need between priorities, workflows, and perspectives between community organizations and healthcare entities. We might envision a future where a provider can bring up information about a patient and immediately see where resources are in a community that might be useful to a given patient compared to where that patient lives and might be able to access them most easily. Consider an example where you observe that a large number of kids playing a sport like baseball seem to suffer from asthma when similar kids playing the same sport in your community did not in previous years. When you add the layer of geography to health assessments, you find that there is a relatively new factory nearby with pollution problems, and the company that owns the factory has been paying residents to help them clean soot and dust off of their homes and vehicles to hide the problem. We need to think more about root causes beyond processes within the body.
Attendees had an opportunity to ask their own questions at the end of the session. The first question pertained to leveraging HIEs and existing connections for closed-loop referrals. In response, panelists explained that standards do not directly apply to some organizations whose data might be useful, such as WIC or daycare facilities. Closed loop referrals help solve healthcare issues, but there is more when you consider a whole person. We are still addressing problems with a medical model, while what we need is a community model.
Another attendee asked about progress on documenting social care interventions in standard ways and associated reimbursement for organizations like Meals on Wheels or other community-based organizations. CalAIM provides reimbursement for multiple types of social services. Processes today still rely on forms, but organizations are increasingly able to map forms to coded standards to make the data useful. We do not always have elegant solutions, but many people are working hard toward extending standard forms into the social services domain.
We should, however, be cautious about relying strictly on codes. If we reward coding, we get more codes, but maybe not the behavior that we really want. For example, do we want people to spend more time working with codes and adding administrative burden that causes people to focus exclusively on codes for the sake of reimbursement, or does doing so lay the same kind of trap that many organizations continue to fall into that limits their ability to push for meaningful progress toward understanding what really drives health equity? More discussion is needed to make sure we incentivize the right work.
Why Regional HIEs are Essential to Close the Health Equity Gap

- Date: Tuesday, August 23, 2022
- Presenters:
- Lynda Rowe, Senior Advisor, Value-based Markets, InterSystems
- Todd Rogow, President & CEO, Healthix
- Nick Bonvino, CEO, Greater Houston Healthconnect
- Overview: Lynda Rowe from InterSystems speaks with Healthix’s Todd Rogow and Greater Houston Healthconnect’s Nick Bonvino about their use of SDOH and, in particular, the value and challenges associated with Z-codes for reporting on SDOH.
Nick Bonvino kicked off this session with an overview of his organization, Greater Houston Healthconnect (GHH). GHH connects 161 hospitals, physician practices, post-acute facilities, clinics, behavioral health centers, and public health departments across 75 counties in the eastern half of Texas and 40 parishes in the western half of Louisiana. The HIE’s services are built on an InterSystems platform that includes value-add tools such as dashboards, mobile applications, data science and machine learning solutions, and services for research and genomics. GHH has expanded its services to provider participants, including closed loop referrals, a “Directory of Community Resources,” refining the handling of patient consent, and integrating clinical and social care data into a Unified Person Record.
 Lynda Rowe serves on the board of an FQHC and talked about the fact that organizations such as the one she works with are still faxing, making many phone calls, and relying on outdated technologies. While HIEs work to provide services that extend to SDOHs, part of the challenge is adapting or helping organizations solve their technology and workflow differences.
Lynda Rowe serves on the board of an FQHC and talked about the fact that organizations such as the one she works with are still faxing, making many phone calls, and relying on outdated technologies. While HIEs work to provide services that extend to SDOHs, part of the challenge is adapting or helping organizations solve their technology and workflow differences.
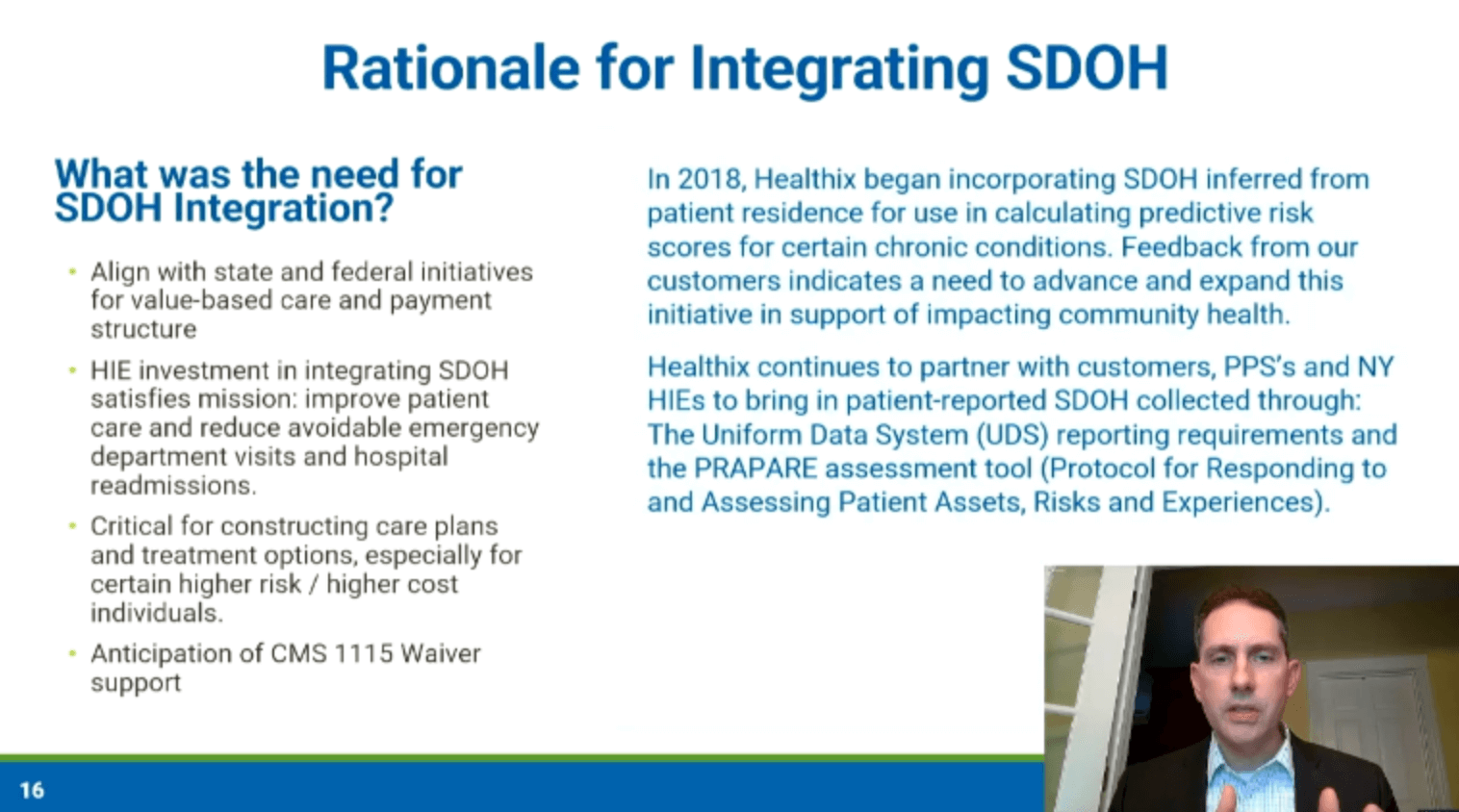
Healthix’s Todd Rogow explained the rationale behind his organization’s efforts to integrate SDOH data into the HIE. In 2018, Healthix began including SDOH, but it was inferred from patient residence for use in calculating predictive risk scores for certain chronic conditions. Today, Healthix continues to expand on this use by partnering with customers, PPSs, and other New York HIEs to incorporate patient-reported SDOH collected through The Uniform Data System (UDS) reporting requirements and the Protocol for Responding to and the Assessing Patient Assets, Risks and Experiences (PRAPARE) assessment tool.
According to Rogow, integrating SDOH data at Healthix meant:
- Better alignment with state and federal initiatives for value-based care and payment structure
- Satisfying Healthix’s mission to improve patient care and avoid ED visits and readmissions
- Supplying data needed for critical care plans and treatment options, especially for certain higher risk, higher cost individuals
- Preparing for CMS 1115 Waiver support
 Healthix has collected over 5.9 million documents pertaining to SDOH, including child care, domestic violence, food insecurity, housing status, poverty, utility bill payment status, education levels, and more. The HIE has been able to realize a lot of value based on the wide variety of data that has been collected over the years. Provider organizations can access curated data through portal views (including SDOH data on a separate tab), SDA transmission to other InterSystems partners, FHIR queries, SDOH alerts, and cross-qualified entity SDOH exchange.
Healthix has collected over 5.9 million documents pertaining to SDOH, including child care, domestic violence, food insecurity, housing status, poverty, utility bill payment status, education levels, and more. The HIE has been able to realize a lot of value based on the wide variety of data that has been collected over the years. Provider organizations can access curated data through portal views (including SDOH data on a separate tab), SDA transmission to other InterSystems partners, FHIR queries, SDOH alerts, and cross-qualified entity SDOH exchange.
Bonvino talked about the move toward whole person care and the pathway to connecting communities for more complete care and planning. GHH recommended the following sequence:
- Establish Trust: Become a trusted system that the community believes in and relies on
- Identify Needs: Identify an individual’s unmet needs through (culturally sensitive) structured assessments, which are then mapped to true needs, strengths, and needs
- Find Available Help: Automatically match needs to services provided by the community (allow for self-referrals)
- Make Connections: Open opportunities to generate referrals from any participating organization
- Measured Progress: Measure performance for populations of interest to see how partners are performing and benefiting
GHH has not figured out all of the details, but Bonvino says that GHH is playing a central role in working with the community to find answers and define and achieve success. Regarding what GHH delivers to partner organizations today—when GHH is queried, consolidated documents are returned, including SDOH data.
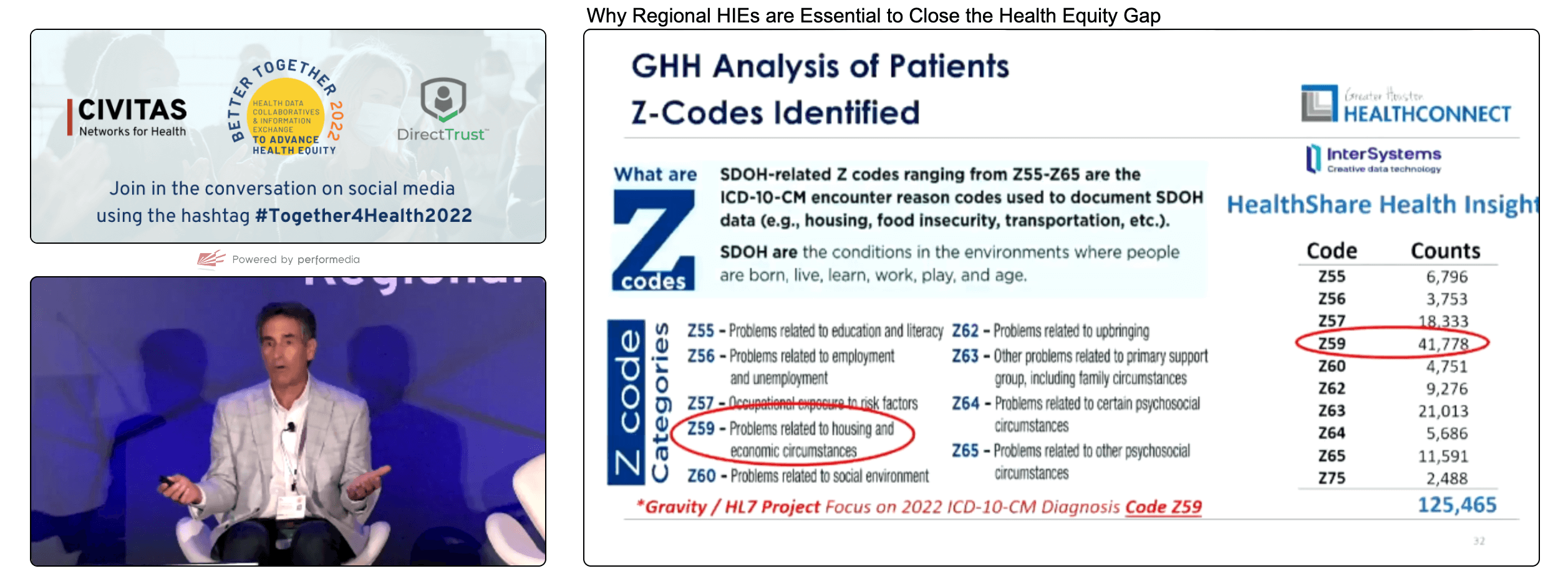
GHH is aligned with the Gravity Project and is currently focused on three risk domains: food insecurity, housing instability, and transportation insecurity. Bonvino said that his team analyzed Z-codes and found the most reported code is Z59 “Problems related to housing and economic circumstances.” It helps to focus an HIE’s work on the most common or pervasive needs. Analyzing data can help make better use of available resources.
In partnership with key stakeholders, GHH is facilitating what Bonvino referred to as The Health Equity Collective, connecting healthcare entities with community based organizations and other information exchange solutions ranging from the United Way to Combined Arms, food banks, and others.
In response to a question about how best to get providers to use Z-codes, Rogow said that there are no secrets from his perspective. Healthix has been fortunate to benefit from robust data and availability of Z-codes, but the HIE has not yet actively promoted their use. Bonvino felt that it can be difficult to get clinicians to code because they are not comfortable asking certain prying questions, and patients do not always feel comfortable answering them. We will have to find ways to move past those uncomfortable feelings to get better and more complete data.
| On Demand | Day One | Day Two | Day Three |
|---|
Thank you for joining us for Day Two of Civitas! Stay tuned for one more day of recaps!
J2 Interactive is an award-winning software development and IT consulting firm specializing in customized solutions for hospitals, labs, research institutions, and health information exchanges.
Our approach to design and development is rooted in a fundamental belief that systems succeed or fail based on how well they serve the people who depend upon them. Drop us a line to learn more.



