| Week One Summary | Week Three Summary | Week Four Summary | Week Five Summary |
|---|

2020 marks the sixth year of SHIEC and the first year of it going virtual! Join us over the next five weeks from August 17 – September 15 as we recap the 10-day series of virtual sessions!
Let’s Innovate, HIEs! Machine Learning and AI
- Date: Tuesday, August 25, 2020
- Presenters:
- Don Woodlock, Vice President of Healthcare Solutions, InterSystems
- Lynda Rowe, Senior Advisor, Value-Based Systems, InterSystems
- Jeff Fried, Director of Product Management – Data Platforms, InterSystems
- Moderator: Moderator: Gary Christensen, General Manager, States, InterSystems
- Overview: InterSystems experts walked viewers through a core understanding of Machine Learning (ML) technology and ways in which ML can be used to improve efficiency and get deeper insights from the increasingly voluminous data sets that HIEs maintain.
For many HIEs, an ROI is difficult to prove but is required to sustain funding. Different groups also value different solutions and share different priorities. For these and other reasons, HIEs must continue to find ways to innovate. InterSystems’ Gary Christensen offered the following conclusions from his experience:
- Think like an entrepreneur. Ten new ideas could result in perhaps one or two viable projects to pursue. The ongoing generation of new ideas is required to get to a few innovations that ultimately stick.
- It is important to find new types of customers, so think more broadly about where your organization’s capabilities could be leveraged.
- Focus on the unique value proposition of your HIE. HIEs tend to have unique access and a unique amount of data in a given region.
The InterSystems team presented information to explain the value of applying Machine Learning to an HIE’s data as one way of identifying opportunities to innovate and bring sellable data products to the forefront.

Don Woodlock, VP of Healthcare Solutions at InterSystems began with a primer on ML and how it works differently from typical data analysis and programming. The main idea is that instead of conducting interviews or coming up with assumed rules to use in a human-built algorithm, ML allows machines to analyze a given set of data, develop inferences, and arrive at conclusions or make predictions based on historical patterns in available information. One major advantage of this approach is that ML solutions can work on massive and complex datasets, whereas traditional analyses are generally more limited. This limitation, in part, is because each iteration and validation of results tends to be a more manual process that requires human intervention, interpretation, and planning.
ML solutions can also self-correct over time and improve as datasets become more robust and inclusive of coordinating data. These automated solutions tend to perform better than having humans come up with the right algorithms through discussions and interviews with Subject Matter Experts (SMEs) or making educated guesses. ML also makes it easier to combine input from a large number of sources to define its rules and come up with data profiles, and tend to use many more features and data points about patients or populations than an individual might think to include.
However, as the presenters noted, there are still critical roles for humans to play in these processes. Ultimately, data scientists are needed to work with data and identify helpful data elements to include, as well as work on defining data models and fine-tuning assumptions. Data scientists also interpret results and discern actionable insights that align with an organization’s mission, budget, and priorities.
Organizations using ML today are moving toward higher levels of automation. One of the major advantages of this move is the ability to have data scientists spend more of their time on high-value data modeling. A larger number of individuals with basic SQL skills, meanwhile, are enabled to execute ML algorithms against new data sets.
ML and AI can be used, for example, to evaluate data to look for anomalies. This evaluation is typically done with time series data to spot changes in patterns, outliers, or exceptions that could be the basis for a solution or special project.
Viewers were directed to an online resource: “IntegratedML: Every SQL Developer is a Data Scientist” for additional information for technical audiences.
The Q&A segment of the session featured a discussion about the importance of iterative approaches to discussions with stakeholders to aid in generating new ideas for products and solutions. There is a trust-building element to achieving success, which often includes bringing stakeholders in to help kick the tires and grow in confidence that a given solution, ML algorithm, or derived data product is accurate and reliable. A final note for HIEs moving in this direction: Experience is showing that it is useful to start ML and AI ventures on lower-criticality questions, such as those that are more administrative in nature. As experience and trust build, organizations can move into the use of ML and AI for questions that have a greater severity weight, such as clinical diagnostics or treatment recommendations.
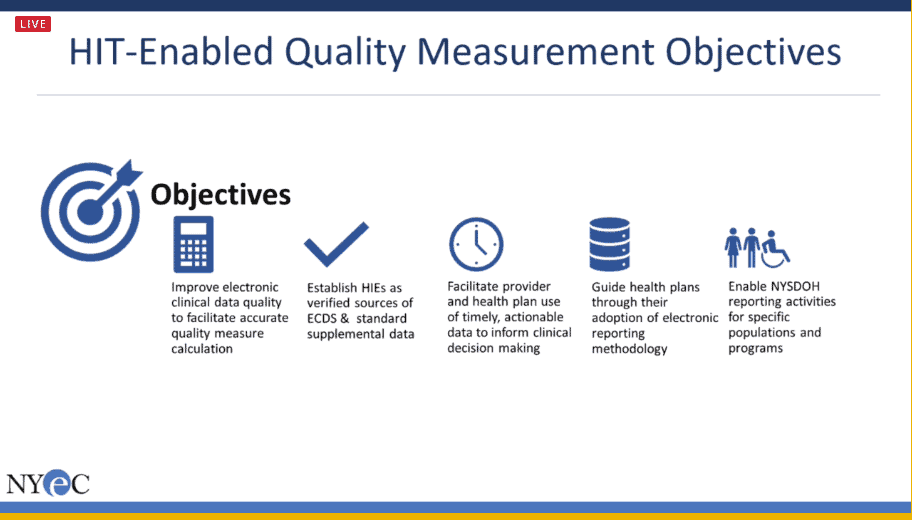
HIE Data Supporting Quality Measurement
- Date: Tuesday, August 25, 2020
- Presenters:
- Preetinder Bassi, Clinical Informatics Manager, New York eHealth Collaborative
- Justin Elliott, Senior Consultant, NYSTEC
- Daniel Porreca, Executive Director, HEALTHeLINK
- Wendy Talbot, Assistant Vice President – Measure Collection and Audit National Committee for Quality Assurance (NCQA)
- Overview: Presenters from New York HIEs and NCQA discussed the role of HIEs in New York as aggregators and validators of data from original sources that serve as the basis for quality measures and reporting.
Approximately 20% of a health plan’s members change plans each year. Furthermore, in Western New York, 73% of patients have medical records in more than one EHR. Because of these moves and segmented records across different systems over time, HIEs are in a prime position to serve as an essential aggregator of data for a given patient or population. It is this aggregator role for longitudinal patient records that serves as the basis for HIEs providing value as a source of quality measurements.
CMS participation was important to the pilot in the Buffalo, NY area. CMS designated Buffalo as a Comprehensive Primary Care Plus (CMC+) medical home region. This designation and direct support for sharing claims data helped to make the program possible.
Justin Elliott from NYSTEC spoke about the role of digital measure specifications, which are machine-readable measures that make interpretation, exchange, and reporting more efficient. NCQA provided three to work with. The pilot program looked at colon and breast cancer screenings in addition to a draft FHIR screening to test high blood pressure. Part of the pilot was identifying data gaps and assessing the readiness of HIE data to provide the necessary information. The colon cancer and breast cancer screening measures proved successful. The high blood pressure example did not proceed because of differences at the time in FHIR standards. The team found that HIEs had some success in this project, but not all machine-readable data could be processed by HIEs.
The researchers found that coding was sufficiently standardized among HIEs, but some data gaps were identified, such as medication fill, hospice, frailty, and certain encounters. New York has created a statewide task force to promote information sharing and assess improvement opportunities based on this and other pilot projects.
Wendy Talbot presented information about HEDIS audits and the burden associated with tracing data back to its original source. NCQA set up a program to attempt to validate data centrally, which could then be shared to satisfy the audit requirements. This effort started in 2019 and seeks to ensure data integrity is maintained from the source and that data aggregators are validated. The goal of this program is to increase access to standard supplemental data, decrease chart chasing, and reduce provider burden and audit burden. Aggregators often have data in different formats. There is a need for added standardization, such as when sharing information with payers and other partners from multiple aggregators.
The original plans did not include medication data because HIEs did not always have information about whether medications were actually dispensed. As the program matures and medication data becomes more consistently available, NCQA does plan to include this type of information for its data validation.
NCQA is currently working on finalizing its pilot. The evaluation criteria developed to test CCDs, data accuracy, and other aspects of data quality ultimately help to relieve the burden for all parties involved in HEDIS audits. Aggregators like HIEs would need to pass both the data ingestion component of the evaluation and the outbound CCD evaluation. These tests are on a pass/fail basis, and if a test fails, feedback is provided to know exactly why it did. The early pilot participants generally took a few attempts to pass these tests, which NCQA considers normal. When an organization passes the validation tests, the aggregator can share data in what NCQA calls standard supplemental data and medical record abstraction.
NCQA is also working on multiple outcome options, such as passing the tests with some caveats. For example, an aggregator might be able to validate on a certain number of data sources but are still working on others, or specific issues are preventing full validation. In these cases, a “validated with exception” result might be granted. The work team is still developing terminology and, following piloting in New York this year, hopes to have a soft launch sometime in the autumn of 2020.
Health Information Exchanges Can Be Vital To Public Health, But They Need To Be Reshaped

- Date: Tuesday, August 25, 2020
- Presenters:
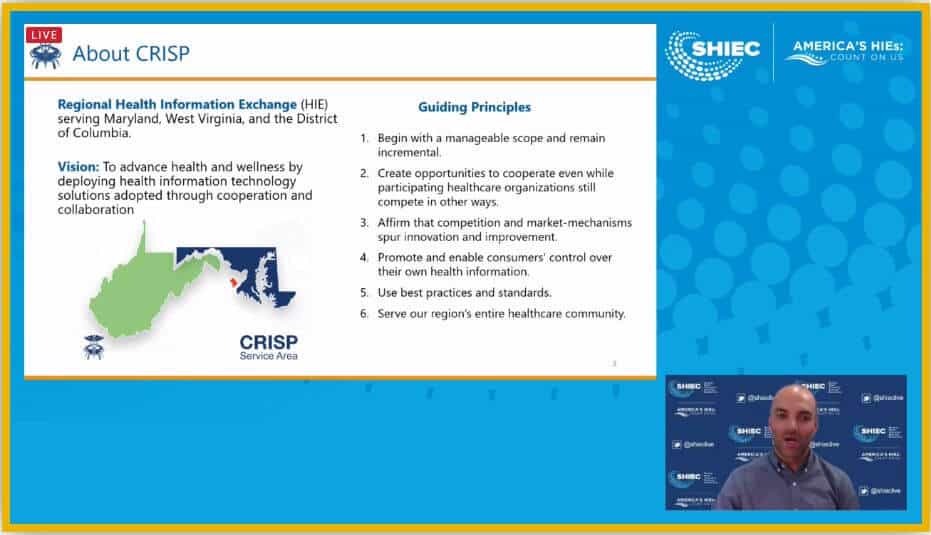
- David Horrocks, President & CEO, Chesapeake Regional Information System for our Patients (CRISP)
- John Kansky, President & CEO, Indiana Health Information Exchange (IHIE)
- Overview: David Horrocks (President and CEO, CRISP) and John Kansky (President and CEO, Indiana Health Information Exchange) discussed the role of HIEs in partnering with states to serve a central role in supporting public health programs. The presenters offered ideas about shifting the perception of HIEs as independent enablers to part of a public-private partnership to viewing them as a service along the lines of a health data utility.
David Horrocks and John Kansky contend that each state should, ideally, have a health data utility, which serves to promote and advance interoperability within and between other states. Such a utility should be based on broad connectivity and standards, as well as be designed in ways that both ensure financial sustainability long-term and promote competition within and between markets. The presenters offered a few different concepts to inform discussions about structuring conversations and coordination efforts:
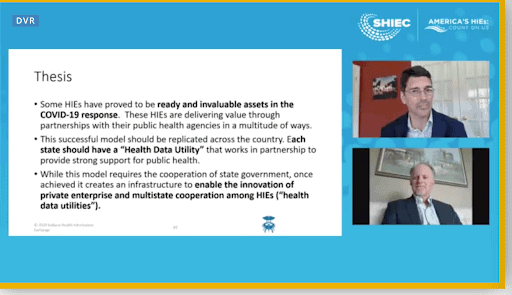
- Concept 1: An HIE’s basic connectivity should function as a state-designated health data utility to which some level of connectivity is mandated (there would be close cooperation with the state).
- Concept 2: HIE organizations should cooperate across state borders through affiliation or consolidation. It is challenging for a given HIE to operate across state borders and still maintain the strongest possible relationship with each state’s government, so affiliations and creative arrangements should be a part of a national structure to both prioritize state needs and provide the greatest level of interstate cooperation.
- Concept 3: Basic clinical document exchange should occur via the future TEFCA-compliant national framework, while HIEs focus on advanced and state-specific needs and value propositions. This aspect will require additional work to carefully design the role of independent HIEs in national and government-supported infrastructure.
- Concept 4: HIEs should cooperate to build a network of interoperable encounter notifications. Real-time alerting is still a cornerstone of HIE value and should be extended through an enhanced network to follow patients as they move, travel, and interact with different entities.
Both Horrocks and Kansky encouraged states to help by identifying gaps that need to be filled to have an acceptable level of service to look and feel like a true utility in the state. In keeping with the theme of public health and government relationship-building this year, this is another great topic for discussion to bring up with state officials and policymakers.
Part 2: HIEs Role in a Pandemic: Supporting Public Health

- Date: Thursday, August 27, 2020
- Presenters:
- Craig Behm, Executive Director, Chesapeake Regional Information System for our Patients (CRISP), MD
- Frances B. Phillips, RN, MHA, Deputy Secretary for Public Health Services, Maryland Department of Health (retired)
- Todd Rogow, President & CEO, Healthix, Inc.
- Overview: CRISP (Maryland) team members discuss the payoff in 2020 of having invested in both infrastructure and key trust-based relationships across the state in the years leading up to the current global pandemic. New York City Department of Public Health and Mental Hygiene’s Jennifer Baumgartner and Healthix (NYC) President and CEO Todd Rogow discuss their respective experiences in one of the country’s first hotbeds of COVID-19 transmission.
Fran Philips and Craig Behm presented a few of CRISP’s collaborative responses to stakeholders’ information needs during the 2020 COVID-19 pandemic. Since CRISP had invested in a strong statewide infrastructure over the past several years, highlighting COVID-19 related data became more of an enhancement exercise than a daunting or seemingly impossible task. Certainly, data gaps and opportunities for improvement existed, but the mechanisms were already largely in place to capture and aggregate laboratory and hospital-level data across the state. The fact that foundational data, connectivity, and use policies were already in place enabled CRISP to rapidly respond to state and public health response requests from the start of the pandemic.
CRISP worked with their stakeholders to understand data needs. They deployed resources and leveraged partnerships to quickly create dashboards that brought pertinent data to the forefront. Fran discussed the fact that the state relied heavily on CRISP’s data and dashboards from the state’s perspective in making closure, safety, and re-opening decisions.
The presenters offered the following examples of value-add solutions delivered by CRISP in partnership with the state of Maryland:
- CRISP enjoys 100% coverage across the state for access to COVID-19 test results. Positive results were pushed to EMS providers and enabling the nearly 1,400 contact tracing resources across the state to dramatically improve and hasten their outreach efforts. For example, in recent weeks, 97% of the approximately 3,000 individuals were contacted within 24 hours of being identified. This kind of rapid response is enabled by CRISP’s existing access to a wide variety of data as well as their investments in data quality to clean specific and necessary data elements such as updated and accurate patient phone numbers.
- Push notifications and various alerts on mobile apps and landing pages were made available to providers across the state for COVID-19 test results in near real-time. These notifications included pilot programs, such as text messages to patients encouraging self-isolation until results are confirmed.
- The Maryland Department of Health identified a strong demand for centralized self-scheduling for drive-through or walk-through testing sites. CRISP was able to repurpose an existing scheduling module to allow physicians to place orders for tests in addition to managing follow-up and scheduling through text messages or email with instructions for self-scheduling at a nearby testing site based on test kit availability. The module also allows for on-site check-in and check-out, accepting walk-ins, and provides pre-populated lab order forms.
- CRISP leveraged its lab feeds to create dynamic dashboards showing test volumes, test completion times, and rates of positive test results. These displays were, and continue to be, used by the state of Maryland and other stakeholders.
- CRISP worked with the Maryland Institute for Emergency Management Services Systems, Maryland Department of Health, and Maryland Hospital Association to consolidate and simplify the daily data submission processes required for hospital bed and COVID-19 case tracking. Dashboards supported surge planning, reducing the federal reporting burden, and proactive hospital resource management.
- CRISP also used its real-time Admission, Discharge, and Transfer (ADT) feeds from participating members to aggregate and display insights into race and ethnicity disparities in access to testing and prevention measures. This information led to evolving public health responses to improve testing rates for vulnerable populations.
The CRISP presenters stressed the importance of remaining nimble and continuing to use their refined data set and tools for new solutions. CRISP is working to finalize data sharing agreements with universities in Maryland to improve rapid contact tracing efforts among student populations as students return to campuses. CRISP will evaluate gaps in the universities’ care alerting and analysis capabilities, especially for child immunizations, and begin to think about how such data integrations can be used to improve flu and COVID-19 intervention programs. Generally speaking, reporting and data product offerings are expected to be a major part of HIEs’ value proposition for the foreseeable future. Fran and Craig echoed the sentiments that we heard last week about the critical role of building relationships with state and public health officials and conveners to identify opportunities for HIEs to continue to deliver value.
Jennifer Baumgartner of the NYC Department of Health and Mental Hygene provided some additional perspective from the public health side of HIE collaborations. COVID-19 surveillance began in January 2020, and data was largely based on Electronic Lab Reporting (ELR) data sets. Jennifer explained that evaluating race, ethnicity, or other potential trends within populations historically required investigating each case. Such an approach soon became impossible after new cases surged to over 1,000 per day in New York City this past spring, proving that new and scalable approaches are needed for public health emergencies like a pandemic.
Public health workers reached out to hospital infection control departments to seek data as an alternative to relying on state registry data. This method also proved unsustainable. Baumgartner’s office had over 50 hospitals to work with, and their respective infection control departments were already overwhelmed. Their experience showed that it was difficult and cumbersome to organize sending lists of patients and essential data to all of the places and offices where it needed to go.
In the spring, public health officials began reaching out to the HIEs serving New York City, looking for automated reports with critical info about hospitalizations, ICU, ventilator use and availability, COVID-19 related admissions and discharges, discharge dispositions, rate, ethnicity, death outcomes, and other important information for guiding response efforts and planning.
Healthix, based in New York City and serving patients across the metro area and beyond, sought ways to support early response efforts by providing patient records to the Javits Field Hospital. The HIE also served as the back-end for New York’s 3-1-1 call service, where residents can inquire about the location and status of loved ones. During this pandemic, this service became an important resource for residents, according to Healthix CEO Todd Rogow, especially since as many as ⅓ of the patients for whom the 3-1-1 service provided information ultimately passed away.
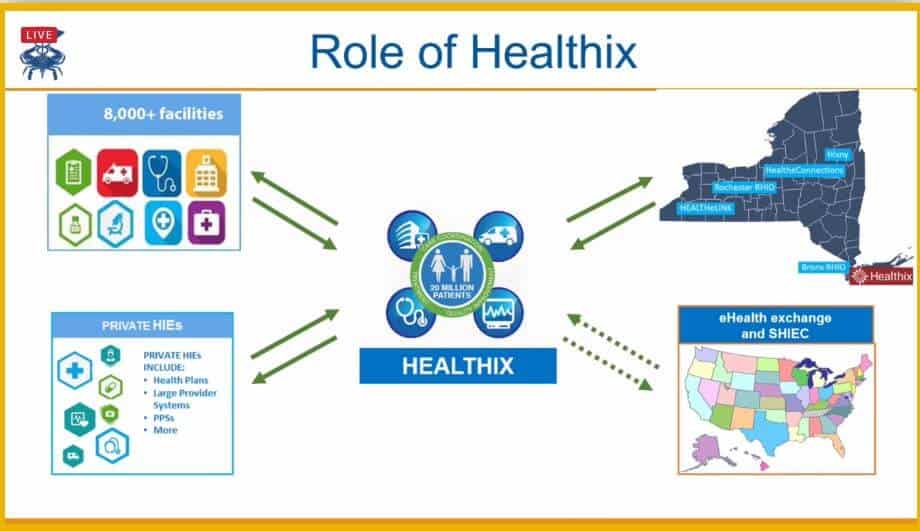
Rogow discussed Healthix’s efforts to facilitate increased COVID-19 test volumes in response to the city government’s goal of expanding from an average of about 20,000 COVID-19 tests per day across the city to 100,000 tests per day. Public health officials are now relying on Healthix to identify high-risk patient populations in the geographic areas it serves. The Healthix team is identifying high-risk patient populations (mostly adults) and those who have not already tested positive for COVID-19. Specifically, they are working to find people that might have difficulty finding testing sites.
In addition to lab test results, Healthix is working to combine census, CDC, and social determinants of health data with clinical data. Predictive models are then applied to this aggregate data to more accurately identify higher-risk patients. More extensive data also helps in identifying why some individuals might be more severely affected by COVID-19.
As we have heard in other SHIEC presentations this year, dashboards and aggregated data visualizations in the form of reports, GIS, or standalone charts have been central to conveying the value of the data to which HIEs have a unique level of access. Interactive, dynamic, and agile dashboards and reports provide direct value to stakeholders at all levels in their own right but also aid in data quality improvement efforts in collaboration with stakeholders.
Clearinghouse Solutions for HIEs

- Date: Thursday, August 27, 2020
- Presenters:
- Matt Hoffman, President & CMIO, UHIN
- Cody Johansen, MPH, Director of Operations, UHIN
- Overview: UHIN leaders discussed their organization’s model to diversify revenue opportunities and improve financial sustainability for their HIE.
Matt Hoffman (President and CMIO) and Cody Johansen (Director of Operations) of UHIN reminded viewers of sustainability concerns for HIEs over the past decade and the progress that HIEs have made to leverage enough revenue opportunities (such as private funding, grants, and membership fees) to build the critical infrastructure needed to be responsive and problem solve flexibly.
UHIN’s approach to diversifying revenue was, in part, to operate as a clearinghouse. Approximately 70% of UHIN’s revenue now comes from the clearinghouse side of their operations, and 30% comes from their HIE services. Only 13% of UHIN’s revenue comes from grants. The general sentiment is that, historically, HIEs have needed to apply for grants to achieve financial stability, even if the nature of some of those grants were not specifically in line with the HIE’s mission or vision. We are starting to see a change in that tendency, and HIEs are increasingly becoming more selective in the funding opportunities they choose to pursue.
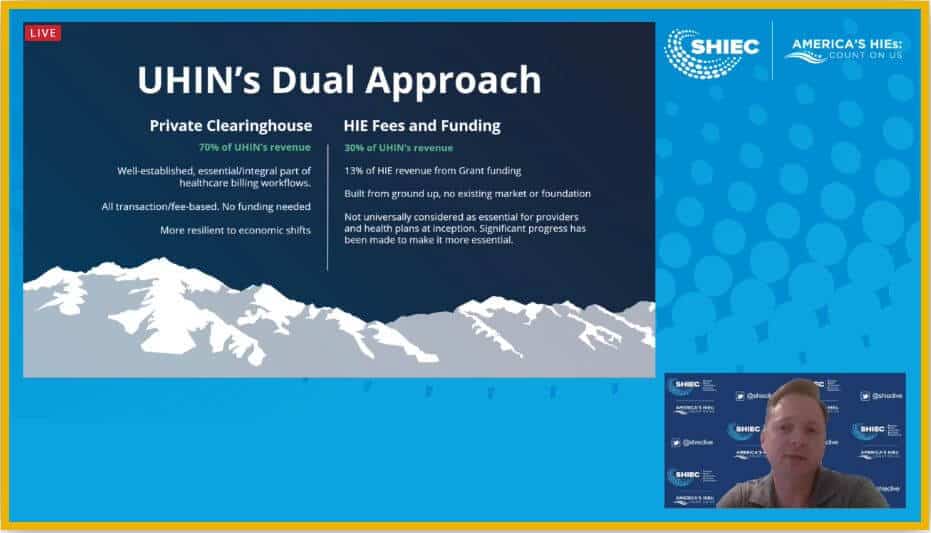
The clearinghouse aspect of UHIN’s revenue model is important because it is based on medical billing, which tends to be more stable over time. This stability provides UHIN with a reliable foundation of funding, which facilitates advancements elsewhere in their organization, including infrastructure efficiencies, data quality improvement based on matching data from both claims and clinical sources, and new types of information available to stakeholders as a result of combining those data sources.
Hoffman provided an example of a company whose business model is to offer drive-through beverage mix-and-match services. They offer customers the ability to mix soda and other beverage flavors to create custom flavor experiences. UHIN and other HIEs are now positioned to begin doing similar kinds of things with data.
Hoffman also discussed the fact that clinical and administrative processes are beginning to merge, and data types are converging with standards that enable data to be combined more easily. There are still challenges, such as with claims data, but progress is being made. While it might not be possible for many HIEs to become or to leverage clearinghouse data directly today, HIEs can still work to move in that direction. Relationship-building and having state leadership that enables and encourages freer affiliations and data use are central to UHIN’s success in pursuing this model.
HIEs should still consider partnering with a clearinghouse, perhaps to offer white-label services to their stakeholders. They also should consider revenue diversification strategies, such as investing more time and energy into building relationships with provider and payer communities, as well as referral programs with financial incentives, to become an essential ingredient in their problem-solving efforts long-term.
An HIE based, In-Workflow Radiation Risk Reduction Program: Approach, Results & Lessons Learned
- Date: Thursday, August 27, 2020
- Presenters:
- James Huizenga, President, CliniCentric
- Alex Vaillancourt, CIO & SVP, Informatics, The Health Collaborative, HealthBridge
- Overview: CliniCentric and The Health Collaborative partnered to introduce a data-driven risk-scoring solution for providers to alert them to cumulative radiation for their patients. Providers use the score to understand how much a patient has had radiation in the past, which informs their decision about studies to order or repeat. The primary goal is to reduce unnecessary duplication in risky and expensive imaging studies. Results so far are positive.
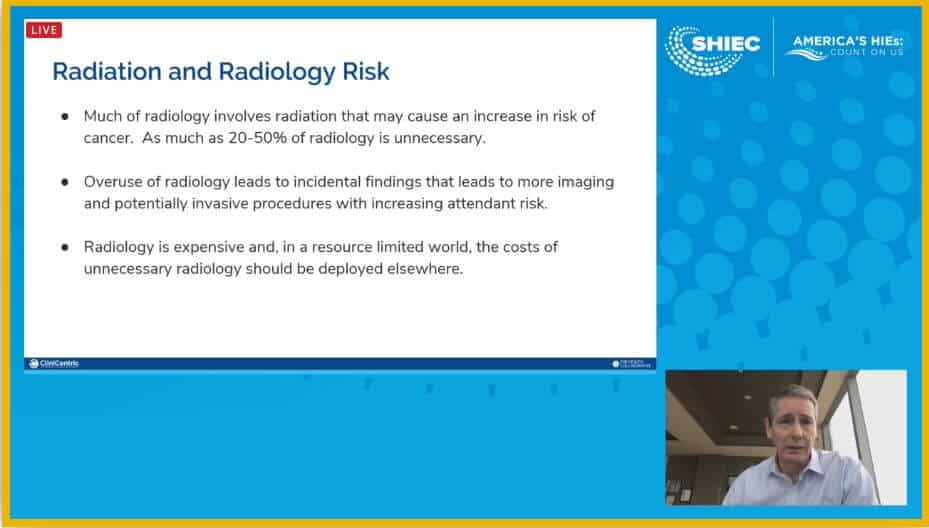
Dr. James Huizenga and Alex Villaincourt presented their work in developing what they term a “RADS” score (Radiation And Diagnostic Study) to aid providers in reducing radiation exposure for patients. As much as 20% to 50% of this exposure is thought to be unnecessary. In addition to the physical health risks associated with the overuse of radiation, there is also the cost to payers. Its overuse could also be considered wasteful in the healthcare system of providing services.
Dr. Huizenga and Villaincourt designed the RADS score to reduce that waste. The RADS score is based on data about a patient’s previous diagnostic or therapeutic radiation exposures and is represented in the form of a three-digit number ranging from 000-999. The higher the score, the higher a patient’s radiation exposure, and the more need there is for a provider to think about whether another study is worth the risk or if alternatives exist for getting the information they need. The presenters talked about future capabilities, such as a provider’s ability to view previous images on-demand in their normal workflow as one alternative to ordering a new study.
The RADS score is displayed conveniently in the header of a patient’s chart, making it easy for a provider to see this information for any patient at any time. There are no additional steps or clicks necessary for a provider to find or view this score.
The benefits of a successful RADS score program include reducing unnecessary radiation, reducing cost, and reducing the number of incidental findings that could result in extensive (and potentially unnecessary) follow-up and burden for the patient.
Project leaders dealt with significant challenges related to combining necessary data from multiple sources across 40 or more hospitals to produce an accurate RADS score. Data quality, data governance, and related work consumed the majority of the time spent on the project. Dr. Huizenga noted that this project also produced related technological improvements, including becoming more efficient or at least partially automating portions of the data quality work and developing new ways of visually presenting information.
Dr. Huizenga offered a few key lessons learned, including the fact that HIEs are well-positioned today to take advantage of and offer these kinds of value-add scores, but will require investments in strong data governance and data normalization work. Ensuring real impact from a project of this type will eventually require some level of automation, so solutions (and the work to support them) should be sustainable, scalable, and cost-effective.
Thank you for joining us this week at SHIEC. Stay tuned for week three’s recap!
| Week One Summary | Week Three Summary | Week Four Summary | Week Five Summary |
|---|
J2 Interactive is an award-winning software development and IT consulting firm with a specialty in customized solutions for HIEs. Read about HIE platform migration.
We would be happy to have a no-obligation discussion about your HIE’s needs with you.



