| Week One Summary | Week Two Summary | Week Four Summary | Week Five Summary |
|---|
2020 marks the sixth year of SHIEC and the first year of it going virtual! Join us over the next five weeks from August 17 – September 15 as we recap the 10-day series of virtual sessions!
FHIRWorx – An Explosion of Information Access
- Date: Tuesday, September 1, 2020
- Presenters:
- Cody Barrette, Director of Data Quality & Visualizations, XchangeWorx
- Prahalad Rangan, Director of Innovation, XchangeWorx
- Joel Ryba, CEO, XchangeWorx
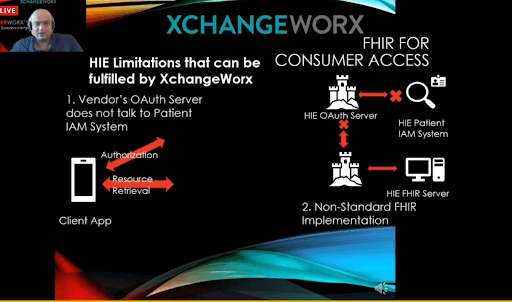
- Overview: The XchangeWorkx team presented how they facilitated a SMART on FHIR application with an HIE to help patients access their own information. The presenters offered examples of the steps they took to leverage OAuth 2.0 in a scenario where an HIE has a patient portal or where no patient portal is offered. XchangeWorkx calls their SMART on FHIR services “FHIRWorx.” Their solution is live at Hixny today.
Prahalad Rangan started the discussion by giving an example of a patient expressing interest in using Apple Health to access their information from an HIE. Traditional information access methods such as CCDAs are too cumbersome in many cases, so using FHIR resources is a useful alternative, provided the application the user chooses is able to consume them.
The basic structure relies on an Identity and Access Management (IAM) system (user directory) that can verify the patient’s credentials and return their HIE ID. The next step is to deploy a token service that can issue OAuth 2.0 tokens through an OAuth 2.0 Authorization Server. An enforcement service is then used to verify the token and validate the patient for whom it was issued. A FHIR resource server is then needed to convert the data available from the HIE into usable resources to return to the patient.
 If an HIE already has a patient portal, the project can be as straightforward as extending the HIE’s IAM (user director) to OAuth 2.0 and enabling the HIE’s data to be served through FHIR resources, which is increasingly a standard capability offered by HIE platforms.
If an HIE already has a patient portal, the project can be as straightforward as extending the HIE’s IAM (user director) to OAuth 2.0 and enabling the HIE’s data to be served through FHIR resources, which is increasingly a standard capability offered by HIE platforms.
If the HIE does not have a patient portal, a few additional steps are required before the above steps can be taken: (1) establishing a user directory, and (2) linking the MPI for users in the directory.
In some cases, HIEs might encounter limitations, which the presenters explained is where XchangeWorx offers additional value. For example, an HIE might have an OAuth 2.0 server that does not communicate with the patient IAM system, or the HIE might have a non-standard FHIR deployment. In the example of Apple Health, the presenters also noted that there are some limitations today with what patients can do. For example, Apple Health works with individual organizations, so patients must log into each organization instead of accessing a single, comprehensive view of their information.
Rangan provided detailed information about the process used to revoke and refresh tokens and the essential role the tokens play in enabling this kind of solution for patients. Walkthroughs were offered, showing the screens used at Hixny.
Cody Barrette presented a use case for getting information back into an EHR. The main reason for building a solution that moves data back into the EHR using FHIR is to avoid requiring providers to step out of their normal workflow to find and access information. Barrette provided an overview of XchangeWorx’s application launch framework leveraging OAuth 2.0 and OpenID Connect. The idea is to enable providers, patients, or other members of a care team to launch SMART on FHIR applications from within (or outside of) software like an EHR. The process works by leveraging tokens to validate the requestor as a known entity. It then passes credentials between software and applications as needed. This process enhances and streamlines the user experience with their EHR without adding steps or logins for the user.
XchangeWorx is currently working on a few new projects, including an application that presents options to discharge nurses about where data should be sent upon a patient’s release. They are also working on a solution to collect patient consent through text or email using SMART on FHIR. The solution sends a message to the patient, and they determine where they want to send their information. Initiatives like these put more control in the hands of patients and care teams so that they can be selective about sending only the most necessary information to those who need it.
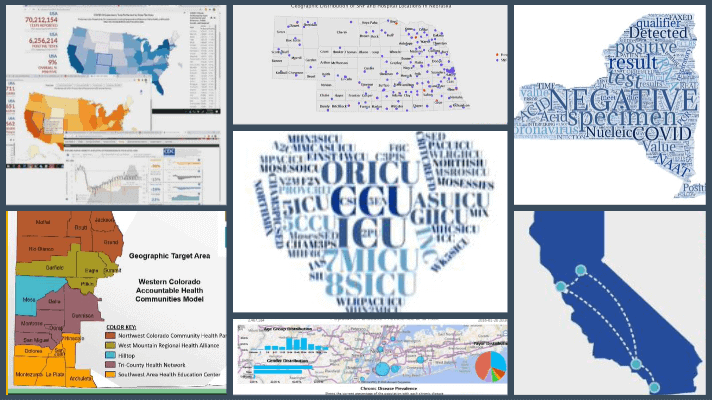
Expanding HIE Capacity to Support Public Health Surveillance Reporting for COVID-19

- Date: Tuesday, September 1, 2020
- Presenters:
- Andrew Fair, Director of Analytics, Bronx RHIO
- Kathy Miller, COO, Bronx RHIO
- Keela Shatzkin, Director of Technical Services, Bronx RHIO/Shatzkin Systems
- Overview: Bronx RHIO leaders presented their experience responding to state data needs during the COVID-19 pandemic and the work required to fill data gaps as efficiently as possible.
Bronx RHIO is one of six qualified entities in New York state. They are HITRUST certified and were recently approved to begin accepting claims data from Medicaid. The RHIO’s geographic coverage extends into Long Island and other parts of New York. As part of the SHIN-NY collaborative, Bronx RHIO shares alerts and CCDs with the other qualified entities and are participating in the Patient Centered Data Home project.
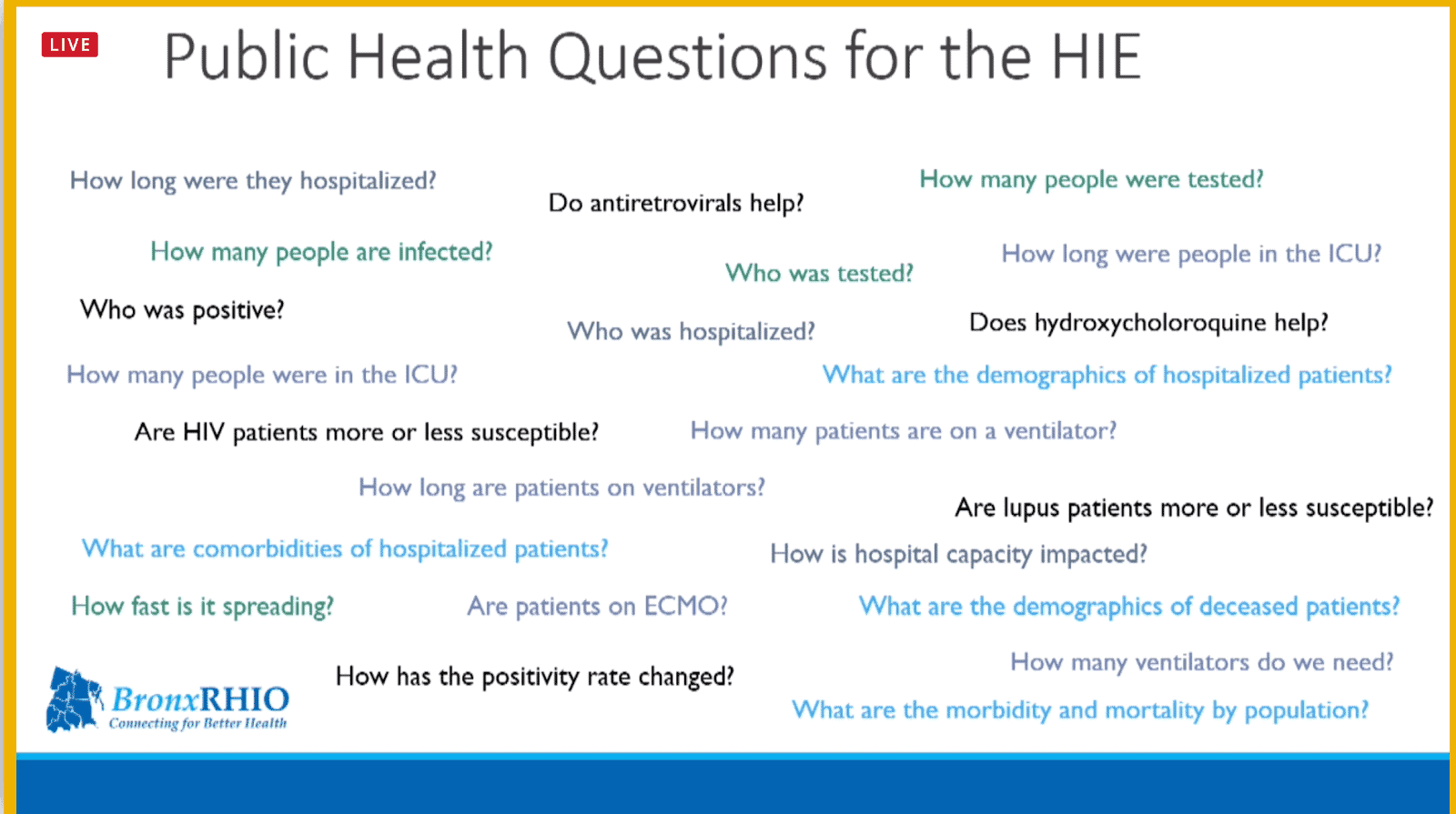
When the pandemic emerged, Bronx RHIO found themselves overwhelmed with questions from external and state agencies. How many people were tested? How many people were infected? How many hospitalized? How long were they hospitalized? Do antiretrovirals help? Are HIV or lupus patients more or less affected? Bronx RHIO received a steady stream of questions like this on daily calls and needed to act quickly to come up with accurate answers.
As the Bronx RHIO team dug into their data to respond to these questions, a number of data quality issues emerged. Specifically, medication data to help show which treatments were more or less effective. They also struggled with data like deceased patients. In some cases, they received data from a source indicating that a patient was deceased, but some time later, the same patient would show up for care elsewhere.
Lab data was also problematic, especially because the clinics and drive-through/walkthrough stations for testing were only interested in capturing a patient’s phone number and were not comprehensive enough with patient demographic data. Some data was better quality but tended to come just from the hospital setting, and other data sources presented greater challenges to bring together. Still, not all hospital-provided data was as useful as they had hoped. One specific example was start and stop times for ventilators.
Since many hospitals temporarily abandoned their ventilator protocols or modified them to respond to the pandemic, Bronx RHIO needed to identify proxies for start and stop times. Ultimately, they found more reliable data and developed a methodology using respiratory flow sheets and examining updates or lack of updates after a certain period of time to signal that a patient was off of a ventilator.
Other information frequently changed, such as the number and capacity of ICU beds. Bronx RHIO worked with its member hospitals to make sure they were included in all update distribution lists to ensure they could report accurate bed counts as ICU beds expanded or were converted.
At the start of the pandemic, standard code sets were problematic in helping to report on specific cases. It took several months before an ICD-10 code was available specifically for COVID-19. Prior to April 2020, which is when the codes were updated, Bronx RHIO had to use a combination of other codes representing coronavirus and extrapolate cases based on matching symptoms. The process of keeping up with constantly changing circumstances, definitions, and approaches took a toll on the team, especially since the stream of questions they needed to answer did not stop.
Fortunately, under a waiver, the state’s Electronic Clinical Laboratory Reporting System was permitted to send positive patient results back out to HIEs. This step was a major benefit that allowed HIEs to improve their daily reporting to the state.
The pandemic and the questions that Bronx RHIO needed to answer have led to improvements in data quality efforts, expansion of data capture initiatives, and a focus on identifying risk factors. For example, using the data that was available to Bronx RHIO, comorbidities were analyzed to look for trends in the number and types of comorbidities that seemed to positively or negatively affect a COVID-19 patient. Bronx RHIO found, for example, that chronic kidney disease, heart disease, and hypertension were associated with significantly higher mortality rates from COVID-19.
Bronx RHIO is now working on enhanced interactive visualizations to improve decision-making and disease monitoring. Projects include interactive dashboards providing insights into COVID-19 testing efforts and geocoding data to provide maps showing the spread of the disease by neighborhood. In addition to these tools, Bronx RHIO is working with the state to de-duplicate and clean data before sending it back. (The Electronic Clinical Laboratory Reporting System does not scrub data for a person with multiple tests or results; each is seen in ECLRs as a new case.)
Looking ahead, the Bronx RHIO team is working to identify patients who are in a “recovery” state and determine the duration of it. They are also assessing the impact of comorbidities on a patient’s recovery, looking at ways to construct the equivalent of an adult vaccination registry for use by contact tracers, schools, and others; and are anticipating needs related to supporting international travel reporting.
Social Information Exchange: Examples and lessons learned from HIEs involved in the CMS AHC model

- Date: Tuesday, September 1, 2020
- Presenters:
- Jennifer Faries, Accountable Health Communities Program Manager and Project Director, MyHealth Access Network, Inc
- Katheryn Jantz, Accountable Health Communities Model Director, Rocky Mountain Health Plans
- David Kendrick, MD, CEO, MyHealth Access Network
- Marc Lassaux, Chief Technology Officer, Quality Health Network
- Overview: MyHealth Access Network, Rocky Mountain Health Plans, and Quality Health Network presented their experiences with the CMS Accountable Health Communities (AHC) model and achieving effective social information exchange.
The need for social information exchange has been gaining momentum at a national level. The presenters explained their respective organizations’ participation in the CMS Account Health Communities (AHC) program and the specific work they have been doing to improve the use of screeners and resource referrals.
MyHealth Access partnered with CMS on a project to determine if identifying and addressing health-related social needs impacts healthcare costs and reduces unnecessary utilization. For their project, MyHealth focused on five core social needs:
- Housing Instability and Quality
- Food Insecurity
- Transportation Needs
- Utility Needs
- Safety/Interpersonal Violence
Jennifer Faries presented a slide showing that as much as 40% of a person’s health and wellbeing is tied to social and economic factors, while the remainder is associated with health behaviors, healthcare delivery, genes and biology, and a person’s physical environment. The social and economic factors category was the largest single contributor.
 In 2016, MyHealth, clinical partners, and community service providers formed what they called the AHC Route 66 Consortium and, in 2018, began screening residents of Oklahoma in Tulsa and Oklahoma Counties for social needs. In 2019, the Route 66 Consortium was granted a state-wide expansion and began screening and providing navigation services to all residents of Oklahoma. MyHealth’s strategy was three-fold:
In 2016, MyHealth, clinical partners, and community service providers formed what they called the AHC Route 66 Consortium and, in 2018, began screening residents of Oklahoma in Tulsa and Oklahoma Counties for social needs. In 2019, the Route 66 Consortium was granted a state-wide expansion and began screening and providing navigation services to all residents of Oklahoma. MyHealth’s strategy was three-fold:
- Partner with six healthcare systems, including more than 90 clinics, care coordination, and hospital locations across Oklahoma.
- Screen everyone and provide custom resource summaries based on home address, regardless of insurance provider.
- Partner with local health departments and care coordination professionals to provide navigation services to eligible Medicaid and Medicare beneficiaries for the CMS partnership.
In the beginning, the screening tool that they used took 15 minutes to complete in person. Few clinics were willing to use it because of the time it took. HIEs provide a unique ability to derive at least some of the needed information, such as leveraging ADT messages in real-time. Certain information can be extracted, such as an up-to-date cell phone number, which can then be used to send text messages to the patient with a link to the screening tool. The text-based version of the screener took 3-5 minutes to complete. The results of the screener are sent to MyHealth, which are then scored. Any individual with an identified Health Related Social Need (HRSN) is provided with a custom referral summary that has details about the referral they need. For Medicare and Medicaid patients, their information is also routed to patient navigators, and they are offered direct support. With this approach, the screener is easy for clinics to use and support. The results of the screeners are also shared with the practices.
Katheryn Jantz provided an overview of the Rocky Mountain Health Plans and Quality Health Network project, which operates through their AHC partnership with CMS. Rocky Mountain Health Plans, a wholly-owned subsidiary of United Healthcare, is a Colorado-based health plan serving Medicaid, Medicare, Child Health Plan Plus, and employer groups.
Quality Health Network was founded in 2004 as a non-profit organization offering secure HIE services in western Colorado. QHN works with physical, behavioral, and social health information.
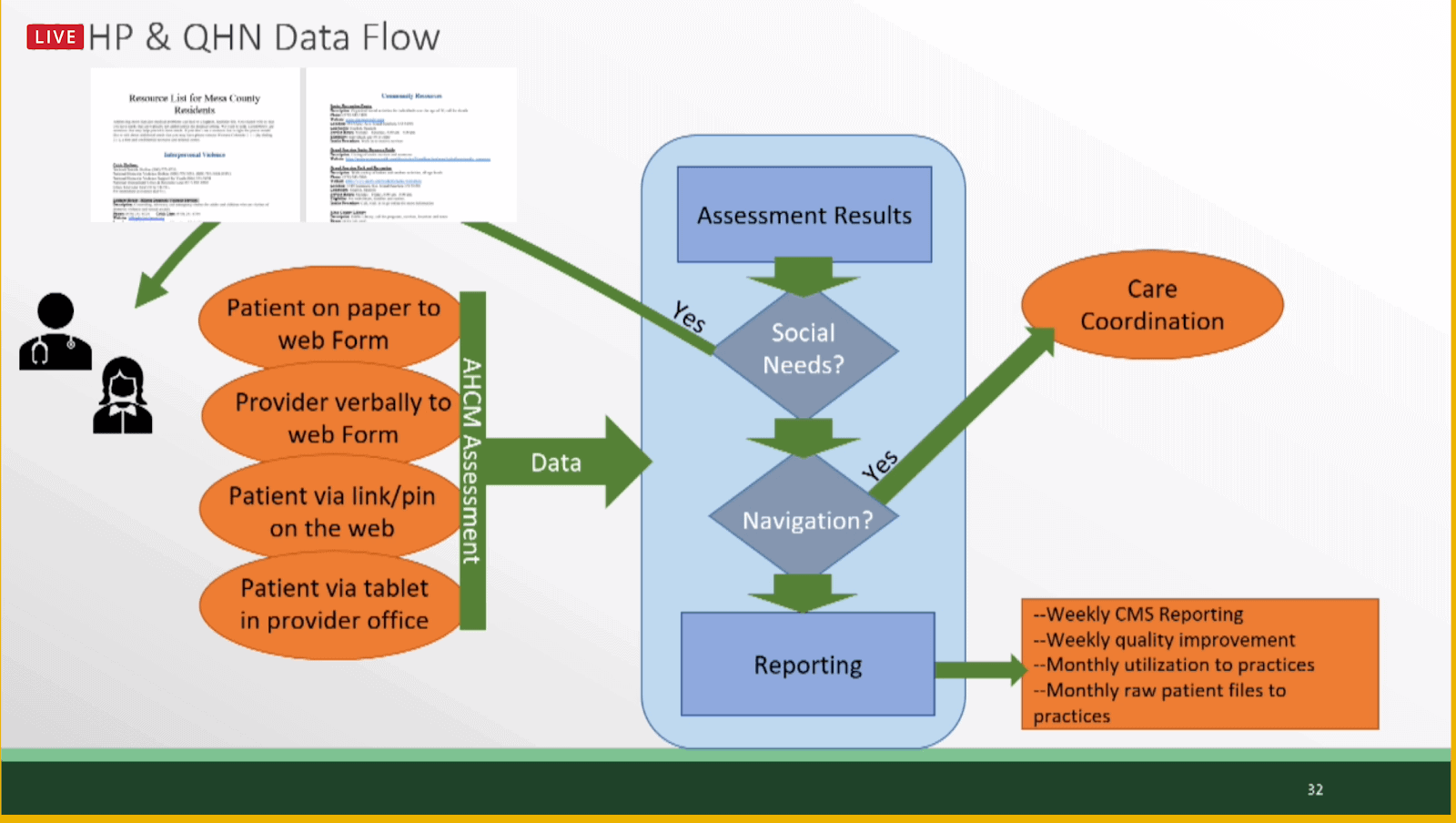
The Colorado project used tablets at the point of care for patients to submit their social needs screeners. Results of the screeners are sent to QHN, where an MPI match takes place, and results are summarized. If a social need is identified, a patient is given a paper resource list at the time of care. As much as technology is improving how we operate in healthcare today, paper remains the simplest way to do things. Paper resources are easy, known, and patients can take it with them, regardless of the level of their technology availability and use. In this example, these are rural or “frontier” clinics, and simpler approaches are preferred. Reporting results and trends to CMS on a weekly basis is a key part of the project.
For the MyHealth program in Oklahoma, results so far are encouraging. The following preliminary tallies help to show the foundation for what is a scalable service and one that is light for clinics and the provider community (i.e., text messages based on ADT messages).
- Over 1 million offers to screen as of August 2020
- 148,000 screener responses
- More than 32,000 responses with an identified need
- 52,000+ individual needs reported
- 2,900+ opened navigation cases
- 3,400+ needs resolved
In western Colorado, the numbers are smaller, but the project started later, the clinics are rural, and the mechanisms of delivery are different.
- 35,000+ screener responses
- 13,690 responses with an identified need
- 26,690 individual needs reported
- 2,640 opened navigation cases
- 1,578 needs resolved
Results so far have provided important insights for the project participants, including the fact that commercially insured patients still report needs and that the wording of the offer to complete a screener significantly affects response rates. (i.e., better results are observed when switching from asking for patient participation to a default position along the lines of “tell us if you do not want us to follow up with you.”)
MyHealth presenters offered the following key lessons learned:
- Mobile screening can be state-wide with the help of HIEs and EHR-agnostic.
- Mobile screening is scalable once adopted.
- Mobile screening is adaptable and can seamlessly transition to telemedicine.
- Details matter with mobile screening, such as area code, shortcode, caller ID, length, and the language used for text messages.
- Mobile screening could be used for many things such as medication reconciliation, depression/anxiety screenings, pre-registration, treatment compliance, and more.
RMHP and QHN offered the following based on their experience so far:
- Keep things simple. If a paper resource list better suits the needs of the population you serve, start there.
- Go slow before you go fast.
- Get the data right. You cannot improve what you cannot see.
- Avoid the pitfalls of offering too many choices. Start with a few simple options.
- Screening is only as good as what you do after the screening. Create a plan for coordination and referrals.
- Be ready to address provider concerns.
To complete the session, presenters offered the following information and responses to questions from viewers:
- It is important to understand the underlying causes of gaps. For example, most food needs are among working adults, and services to support them are often only open during normal business hours. There might be opportunities to address these disconnects by offering extended hours or incorporating a food bank into a clinic location.
- While some might wonder about whether elderly patients have or respond to text messages, their experience so far has shown that even if a patient does not have a cell phone, a caregiver accompanying them usually does. To date, in Oklahoma, staff report over 80% success rate in delivering a link to a mobile device. Oklahoma offered a way for caregivers to complete the screener on behalf of a patient. The presenters acknowledged that it is difficult to get to everyone, but delivery and response rates so far are promising.
- There will be details to work through, such as each phone service carrier having different limits on the number of characters permitted in a text message. The presenters recommend collaborating with an expert on this topic to structure the messages and screeners in a way that it works across carriers.
- There is a strong desire to collaborate between clinics and resources in both Oklahoma and western Colorado. In Oklahoma, results are shared with all stakeholders involved in a patient’s care. In western Colorado, additional data elements were added, such as the clinic where the screener was taken, to enable coordination between clinic sites as patients sought care at different facilities.
- When using text messages, relationships and how screeners are introduced to patients are critically important. If not introduced properly or at the right time, a text message could look like spam or simply be ignored. Having a relationship with the patient and educating them about the text message and its value to them and their care team makes all the difference. This introduction is somewhat less of a factor when using a mobile device at the point of care. However, it is still important to have a well-scripted method of introducing the value of the patient taking the time to complete a screener.
Federal Agency HIE Value Panel

- Date: Thursday, September 3, 2020
- Presenters:
- Cindy Pan, VHIE Program Manager, U.S. Department of Veterans Affairs
- Denise St. Clair, Ph.D., Health Informatics and Interoperability Group (HIIG), Office of Burden Reduction and Health Informatics (OBRHI), Centers for Medicare & Medicaid Services (CMS)
- Moderator: Timothy Ohrum, Grassroots & External Relations Advisor, SHIEC
- Overview: Cindy Pan and Denise St. Clair discussed their respective federal departments’ initiatives and how HIEs are, and can become, involved.
Denise St. Clair began the session by introducing CMS’ new Office of Burden Reduction and Health Informatics. Under the leadership of Dr. Mary Greene, the goal of this new office is to unify CMS’ efforts to reduce regulatory and administrative burdens for beneficiaries and the medical community.
A significant amount of time and effort has been invested in understanding the pain points that lead to the perception of provider burden and burnout. This investigation was part of an initiative known as “Patients over Paperwork.” Historically, the fragmented and data quality issues that HIEs have been working through made the top of the list. However, today, that has shifted to pre-authorization, which is now the top contributor to the potentially avoidable burden.
St. Clair described three main focus areas at CMS:
- Empowering patients to access their own health information, safely and securely, to make the best-informed decisions about their care.
- Connecting healthcare through seamless data exchange across the care continuum.
- Promoting the use of the latest technology and standards to drive innovation and data exchange in healthcare.
The Patient Access final rule will require payers to make APIs available to access information. The intent of APIs is to empower patients to access their information in right-sized quantities instead of forcing them to read through long lists of information to find what they need. Patients must be the ones to initiate requests through their preferred apps.
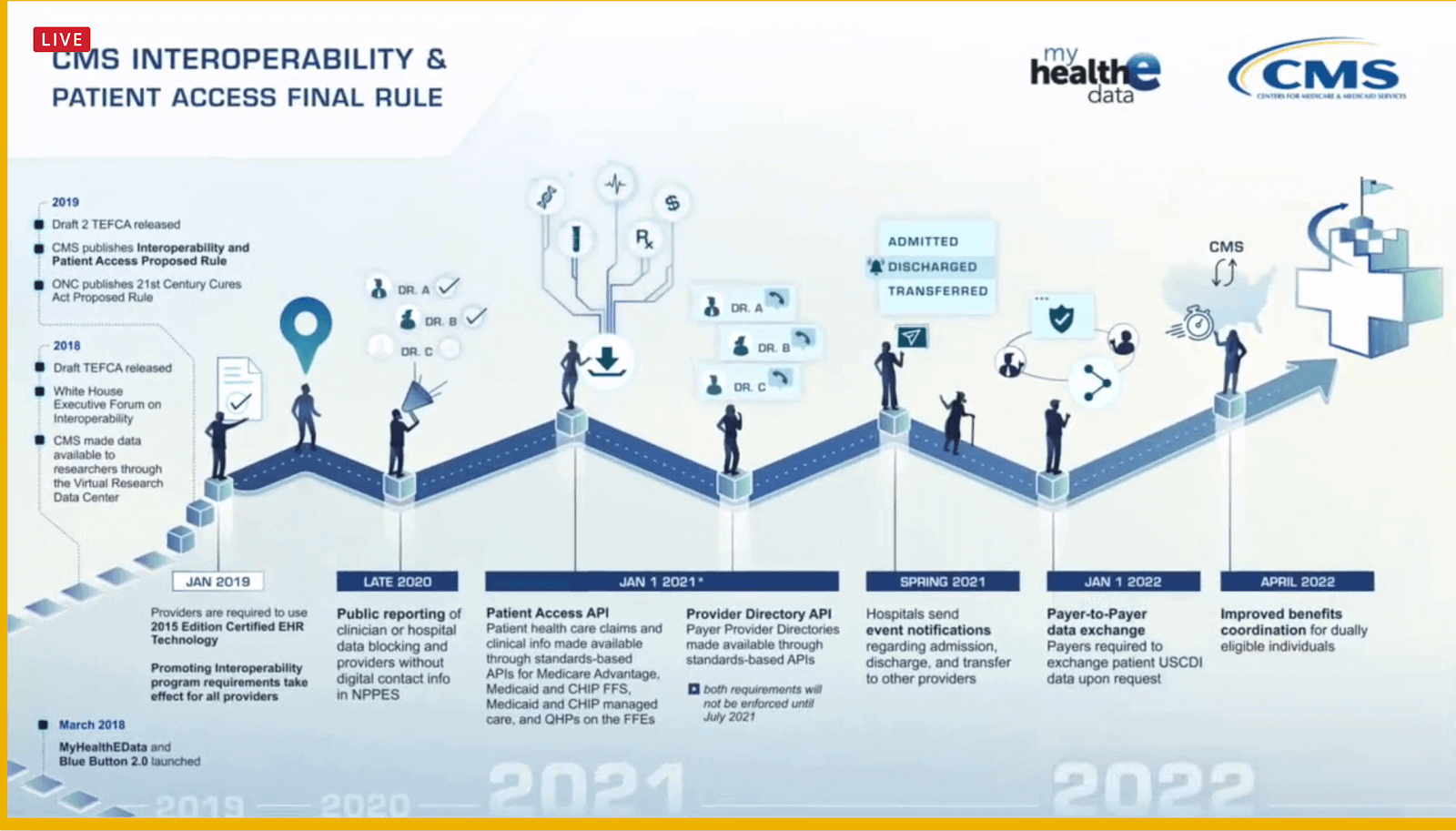 The rule also describes the role intermediaries can play in facilitating patient encounter notifications in the form of Admission, Discharge, and Transfer (ADT) messages.
The rule also describes the role intermediaries can play in facilitating patient encounter notifications in the form of Admission, Discharge, and Transfer (ADT) messages.
Cindy Pan then described her work on the new federal joint HIE between the VA, Department of Defense, and the U.S. Coast Guard. Over the past two years, she and her colleagues have been working through many of the challenges that HIEs know well. A critical catalyst for this joint HIE was the Mission Act, which, in part, allowed the VA to move from an opt-in model to an opt-out consent model. It took approximately ten years, but now all VA patients are opted in by default. This accomplishment has made a major difference in accelerating the value of HIE at the federal level. In the past, about 600,000 of the roughly 6 million patients followed by the VA were opted-in. Since the Mission Act took effect and all are opted-in by default, only about 2,000 have elected to opt-out.
The VA had formerly been connected to other HIEs, and the new joint partnership will seek to further develop this effort. The joint HIE initiative will focus on expanding connectivity with as many partners as possible. Work is underway to complete connections to Commonwell and Carequality to make connections as easy as possible for the largest number of partners. Based on their research so far, it does not look like there is significant overlap between the various services. They are expecting a different group of partners from each connection and plan to connect to all of them, in addition to eHealth Exchange.
One of the side-effects of this robust expansion, however, is a more thorough and time-consuming onboarding process. The joint HIE is limited to five onboarding projects at a time. Any HIEs not currently connected are encouraged to contact Pan or her department to start the process as soon as possible.
Eric Manders from the CDC Center for Global Health spoke about the strong interest in HIE internationally. Eric’s department helps convey lessons learned from U.S. HIE efforts to share with other countries to inform their HIE plans and policies, while also scanning other countries’ programs for valuable insights that can be used in the U.S.
In broad terms, the government is asking HIEs to think creatively about the kinds of data they can add or develop about patients from various sources to enhance the value of the Patient Access API and others. Long-term, a patient should be able to get their full medical record from birth to death on a device and in a way that they can truly understand it and it follows them as they move throughout the healthcare ecosystem.
How HIEs Can Use Claims Data to Support Value-based Programs

- Date: Thursday, September 3, 2020
- Presenters:
- John Ezzard, Specialist Leader, Deloitte
- Craig Jones, Program Advisor and Consultant, Capitol Health Associates
- David Kendrick, MD, CEO, MyHealth Access Network
- Anne Santifer, Director of Health Information Technology, Arkansas Department of Health
- Richard Shonk, MD, Chief Medical Officer, The Health Collaborative
- Overview: Panelists discussed the vital role that HIEs play as a trusted, neutral territory between payers and providers, and the value derived from cleaning and blending clinical and claims data as a better representation of both patient and population.
Increasingly, HIEs are being encouraged to go beyond being HIEs and create Health Information Ecosystems where multiple data sources can come together. Such an initiative would enable providers to take on risks safely, with greater understanding. Patients could also benefit from more robust information in their hands and the hands of their care team members.
Panelists discussed the historical significance of gaps between payers and providers when it comes to data and the extent to which providers have felt they can trust data from payers. Payers have asked HIEs to begin incorporating claims data, in part to help position the claims data more neutrally in conversations with providers. HIEs have been working diligently to clean, improve, and augment data for years, so this work is a natural extension of what HIEs are already accustomed to doing. Having HIEs serve as a neutral third party helps to get past questions of trust and move on to substantive discussions about improvement opportunities.
A major part of the value proposition is facilitating and engaging with different groups where conversations have not taken place before. For example, as the trusted third party, HIEs begin to have better discussions with payers about what the data shows from a claims and clinical data perspective. The HIEs can serve as a convener to bring providers to the table to talk about what the HIEs are finding in collaboration with payers and discuss using their data. This multi-faceted sharing of new observations creates a foundation for deeper cooperation and relationship-building.
 There are certain limitations to claims data that must be acknowledged. Due to the 3-6 month lag, claims data should be viewed as a supplemental data set to provide more information about a patient to help with both care and providers assuming more risk in value-based care programs. Claims data must also be normalized and presented in a trustworthy way instead of contradictory and confusing. Investing in a “coach” type role at the HIE level helps clinicians build trust in the data and make sense of which information is most relevant and worth a provider’s time to review. Claims data also does not capture non-Fee-For-Service encounters consistently, so it should not necessarily be used by itself at the HIE level.
There are certain limitations to claims data that must be acknowledged. Due to the 3-6 month lag, claims data should be viewed as a supplemental data set to provide more information about a patient to help with both care and providers assuming more risk in value-based care programs. Claims data must also be normalized and presented in a trustworthy way instead of contradictory and confusing. Investing in a “coach” type role at the HIE level helps clinicians build trust in the data and make sense of which information is most relevant and worth a provider’s time to review. Claims data also does not capture non-Fee-For-Service encounters consistently, so it should not necessarily be used by itself at the HIE level.
HIEs have the ability to help frame the data in ways that provide the highest value to providers. This can be in the form of customized reports that match the level of a provider’s sophistication and requirements in reviewing the data, to the value offered by HIEs in engaging “coaches” to help interpret measurements and trends with and on behalf of the providers. That translation layer is an essential role that HIEs play.
Claims data provides some advantages over other data types, not only in better outlining a patient’s history and the costs associated with their required care but also in attributions and clarity on death causes vital when analyzing deceased COVID-19 patients.
Identity management is still a basic service that HIEs can provide to blend data. In addition to claims data, HIEs should continue to identify and bring in data from other sources such as EMS and public health data. The more diverse data an HIE can provide, the better. Providing that data with heightened attention to quality and coaching services for practices to get the most value out of the full breadth of information available is a combination that leads to success in building trust over time. It does take time, but consistent efforts to engage, communicate, and include payers and providers in the HIE’s data governance program are paying off.
Leveraging HIE to Support State Health Department During COVID-19 Pandemic and Beyond
- Date: Thursday, September 3, 2020
- Presenters:
- Joe Kachelski, CEO, Wisconsin Statewide Health Information Network (WISHIN)
- Steve Rottmann, COO, Wisconsin Statewide Health Information Network (WISHIN)
- Christopher Sell, Section Chief, Informatics Architecture Section, Division of Public Health – Wisconsin
- Renee Towne, Director of Quality Programs, KPI Ninja
- Overview: Leaders from WISHIN, the Wisconsin Division of Public Health, and KPI Ninja presented their work in responding to data needs related to the COVID-19 pandemic.
The Wisconsin Division of Public Health requested health data related to COVID-19 to assist decision-makers in the outbreak response. There was an urgent need for cross-community, patient-identifiable health data to inform the state’s pandemic response and look for opportunities to link this data to other DPH data sources to augment decision support at the state level. The partnership’s initial goal was to put in place daily rosters sent to the Division of Public Health that met COVID-like, COVID-positive, COVID-recovered, and COVID-deceased criteria.
The state partnered with WISHIN to supply the technical infrastructure. Funding for data projects was limited, but the need was still apparent, so partnerships made sense. Specifically, the DPH was looking for patient demographics, procedures, vitals, lab results, medications, encounter information, and the equipment used in interventions. The desire was to combine this data with existing data available from various DPH repositories to fill gaps.
By the end of May, they had the needed data feed set up, but it was not clear at the time how much time and effort it would take to work with the newly available data. This first wave of activity to pair WISHIN and DPH data comprised Phase 1 of the project.
From WISHIN and KPI Ninja’s perspective, a significant amount of time and effort would be spent assessing the existing infrastructure, identifying data strengths and opportunities, and unlocking useful data contained in HL7 messages and parsed data from CCDAs. These efforts would become Phase 2.
As part of this infrastructure modernization work, several critical items emerged, including the need to:
- Merge HL7v2 and CCDA into a Unified Data Model
- Support queries based on COVID-19 business needs across the WISHIN network
- Enhance enforcement of file content and formatting, per specifications
The participating teams at WISHIN and KPI Ninja adopted an agile and iterative approach to producing and improving data/reports every few weeks as needs and priorities evolved while the pandemic played out.
Phase 3 of this initiative was to automate WISHIN files, including COVID-19 rosters, as part of a unified data model with defined parameters, with pertinent information about these patients sent to the Wisconsin Division of Public Health on a daily basis.
The presenters listed the following major outcomes from the COVID-19 response initiative in Wisconsin. The response:
- Enabled officials to monitor and analyze a COVID-19 patient’s journey over time due to daily rosters
- Established a new data sharing and augmentation pilot between WISHIN and the Wisconsin DPH.
- Identified empirical discrepancies in data submission workflows across the network.
- Gave the ability to compare the COVID-like cohort and potential COVID-19 cases with confirmed lab results.
- Improved WISHIN’s infrastructure, which will convey benefits for its other stakeholders.
- Provided a foundation for a long-term collaborative relationship between WISHIN and the Wisconsin DPH to facilitate future work and public health response initiatives.
The presenters offered a few lessons learned:
- Contractual requirements for work engagement can be difficult with compressed timelines.
- Data can vary greatly from one source to another.
- The right partner is needed to parse and aggregate the data in an intelligible manner.
- Initial data validation can be challenging and resource-intensive.
- HIEs have the potential to be a single source of truth, not only during the COVID-19 pandemic but also in future disease outbreaks, and they should consider positioning themselves accordingly.
| Week One Summary | Week Two Summary | Week Four Summary | Week Five Summary |
|---|
Thank you for joining us this week at SHIEC. Stay tuned for week four’s recap!
J2 Interactive is an award-winning software development and IT consulting firm with a specialty in customized solutions for HIEs. Read about HIE platform migration.
We would be happy to have a no-obligation discussion about your HIE’s needs with you.



